Glandular hyperplasia of the endometrium is a serious pathology, which is characterized by abnormal proliferation of tissues of the uterine layer. Some of the forms of the disease, including atypical and focal, are considered a precancerous condition. For this reason, delaying treatment is strictly prohibited.
Characteristic
Endometrial hyperplasia is a pathology that affects the entire genitourinary system. As it develops, the uterine tissue grows, becomes thicker and denser, thereby increasing the risk of cells transforming into malignant ones. Especially in cases where atypical or complex hyperplasia is detected. Pathology is diagnosed in women of different age categories.
The peculiarity of this disease is that it affects not only the reproductive, but also the immune, nervous, and endocrine systems.
There are several reasons why the pathological process begins. The most important of them is hormonal disorders. The disease develops under the influence of the following factors:
-
- early or excessively late onset of regulation;
- no history of childbirth;
- disruptions in the functioning of the endocrine system;
- disruption of communication between the pituitary gland and hypothalamus;
- exposure to stress;
- ovarian cyst;
- carrying out abortion procedures;
- immunosuppression;
- the presence of infectious diseases in the genitourinary system that occur in a chronic form;
- use of an intrauterine device;
- presence of bad habits;
- excessive body weight;
- diseases of the biliary tract, liver and gastrointestinal tract;
- hypertension;
- uncontrolled use of oral contraception.
These factors have a particular influence with the onset of menopause, but even at a younger age, women are not immune from the development of pathology.
Symptoms
Glandular hyperplasia is a pathology in which abnormal proliferation of endometrial cells occurs. Most often it is observed after 40 years. Due to the fact that the onset of pathological changes is provoked by hormonal imbalance, the disease is characterized by the following clinical manifestations:
- heavy bleeding not only during the regular period, but also in other phases of the cycle;
- pronounced pain syndrome during critical days;
- dizziness and general deterioration;
- a sharp decrease in body weight;
- menstruation with clots;
- cycle failure.
Classification
There are several types of the disease:
- simple glandular hyperplasia without atypia;
- glandular-cystic;
- cystic;
- basal;
- atypical;
- diffuse;
- focal;
- endometrial polyps.
Regardless of the type of pathology, menstruation becomes more painful, and problems with conception arise. To determine the type of hyperplasia, a comprehensive diagnosis of the disease is carried out. The diagnosis is made based on the data obtained.
Glandular
With this form of the disease, the internal mucous tissues of the reproductive organ are damaged. The affected cells begin to increase in size and number, but their structure does not undergo pathological changes. Over time, the boundaries between the permanent and replacement layers are erased.
The main signs of the development of pathology are acyclic bleeding from the uterus. This type of disease is much easier to treat than focal glandular endometrial hyperplasia.
Glandular-cystic
The disease begins to develop due to excessive concentrations of estrogen and lack of progesterone. Similar disorders occur with ovarian cystosis, lack of ovulation and the presence of hormone-producing tumors of the appendages. The glands stop functioning normally.
Glandular-cystic pathology is characterized by cystosis of the glandular tissues of the uterus. The neoplasms are small, and fluid containing a lot of estrogen accumulates in them.
Cystic
With the development of this pathology, the glands increase in size and volume, but not in quantity, after which they transform into cysts. The basal layer is not separated from the functional one. Discharge in the form of blood becomes pathological, acyclic bleeding appears, the menstrual cycle and reproductive function are disrupted.
Basal
This pathology is diagnosed quite rarely. The cause of its development is often inflammatory processes in the vagina or uterus. The disease leads to excessive growth of the glands of the basal layer and the appearance of fairly large polymorphic nuclei of stromal cells.
Initially, the pathology occurs without discharge outside the regulative period. Later, prolonged and painful menstruation and acyclic bleeding begin to occur.
Atypical
Atypical endometrial hyperplasia is the most dangerous of all forms of the disease. As a result of its development, the cells of the mucous layer of the uterus grow abnormally. The endometrium stops changing during the cycle. The tissues of the uterus begin to degenerate into malignant ones.
Diffuse
With this disease, proliferative processes begin, covering endometrial tissue over its entire surface. Pathology manifests itself in the form of proliferation of glands and the appearance of cysts, spreading to all areas of the mucous membranes.
The development of a diffuse type of disease can be provoked by a uterine polyp, inflammatory processes in the reproductive organ, frequent abortive measures, hormonal fluctuations and disorders of the endocrine system. As a result of the onset of the pathological process, menstruation becomes profuse and painful.
Focal
The disease provokes changes in the mucous layer of the uterus and cycle failure. When the secretory phase begins, the endometrium reaches its maximum thickness.
At the same time, its cells grow unevenly and provoke the appearance of polyps. These, in turn, transform into cysts, which, if left untreated, mutate into malignant formations.
In advanced forms of focal pathology, radical measures are taken - the reproductive organ is completely removed.
Endometrial polyps
Endometrial tissue polyps are clots on which light pink blisters appear. Just like uterine fibroids, this pathology is asymptomatic at the initial stage. Neoplasms can vary in shape and size.
The tissues of the uterine layer grow excessively quickly. Often polyps have a thin stalk, but can grow directly from the endometrium itself.
The pathology is prone to frequent relapses, especially in women after 50 years, when the concentration of sex hormones decreases significantly.
Possibility of getting pregnant
Even with simple glandular hyperplasia, getting pregnant is very problematic and extremely undesirable. Ovulation in the process of development of pathology is disrupted, the duration of menstruation changes.
Due to excessive growth of the mucous tissues of the reproductive organ, the egg cannot be implanted and infertility occurs. Even if conception occurs, the outcome will be unfavorable. Often it ends in spontaneous abortion.
Serious abnormalities in fetal development are also possible.
Pregnancy with hyperplasia can lead to active growth of polyps in the ovaries and uterus, as well as their mutation into malignant formations.
Diagnostic methods
In order to identify hyperplasia and determine its type, a number of diagnostic measures are carried out:
- Ultrasound;
- hysteroscopy;
- scraping.
Only after making an accurate diagnosis can the optimal course of treatment be selected.
Ultrasound
The study is carried out transvaginally between menstruation. In this case, it is possible to identify changes in the tissues of the uterus, determine their severity and scale. Ultrasound gives an accurate idea of the degree of thickening of the layer of the reproductive organ, the presence of nodes, cysts and polyps. As a result, not only pathology is detected, but also information appears about the condition of nearby organs.
Scraping
Ultrasound examination fails to identify structural and morphological changes that the uterine mucosa has undergone. For this reason, they resort to diagnostic curettage.
A special loop or curette is inserted into the vaginal cavity, and then all necessary manipulations are carried out in the cervical canal and the cavity of the reproductive organ.
The obtained biomaterials are transferred for subsequent laboratory research.
Hysteroscopy
This is an effective method of examining the cervix and the cavity of the reproductive organ, which uses a special device - a hysteroscope.
In addition to a visual examination to identify glandular hyperplasia, tissue is collected and sent for further research. In this way, it is possible to accurately determine the type of pathology.
To obtain reliable results, the procedure is carried out closer to the arrival of critical days.
This method is considered the most effective among all others. The accuracy of the results reaches 95%.
Treatment regimen
The choice of treatment tactics for glandular endometrial hyperplasia depends on many factors, including the woman’s age, features of the clinical picture, a history of concomitant pathologies and the form of the disease. The selection of drugs should be carried out exclusively by a doctor. In some cases, it is not possible to do without surgical intervention.
Among the basic principles of treatment are the following:
- the use of special means to stop uterine bleeding;
- restoration of the menstrual cycle or acceleration of the process of atrophic changes;
- relapse prevention.
If pathology is detected during puberty, the treatment regimen is as follows:
- General restorative and hemostatic therapy (Oxytocin, Vikasol, vitamin-mineral complexes and preparations containing iron).
- Hormonal drugs (Rigevidon, Marvelon).
- If there is no proper effect from drug therapy, curettage is performed inside the cervix and reproductive organ.
If the pathology begins to develop in a woman of reproductive age, then after all diagnostic measures have been carried out, hormonal therapy is prescribed using medications such as Norethisterone or Danazol.
If the desired effect is not achieved, surgical intervention is resorted to. In case of polycystic disease, resection of the appendages is performed, and if hormone-producing tumors are detected, the ovaries are removed.
Pregnancy in the future becomes impossible.
During menopause, hysteroscopy is first performed. Depending on the results obtained during the study, hormonal medications or surgery may be prescribed.
Pathology that develops during menopause is usually treated by expiration of the reproductive organ and ovaries. Hormonal treatment is possible only in the case of primary glandular hyperplasia.
Glandular hyperplasia is a dangerous disease that requires immediate treatment. The problem with this is that it is often asymptomatic at the initial stage of development and is diagnosed quite late, when the scale of the lesion is already quite large.
Serious complications that pathology provokes are infertility and transformation into a malignant formation. This determines the need for rapid elimination of the pathological process.
With timely initiation and correctly selected therapy, the activity of the reproductive system can most often be completely restored.
Source: https://TopGinekolog.ru/bolezni/zhelezistaya-giperplaziya-endometriya
Glandular hyperplasia of the endometrium: causes, diagnosis, principles of treatment
Among patients under 45 years of age who applied to medical institutions for reproductive function disorders, endometrium with glandular hyperplasia is detected in 6.6%, and among women who have polycystic ovary syndrome, the risk of developing hyperplasia of the uterine mucosa, according to various sources, ranges from 75 to 90%.
Despite numerous studies in the field of studying the mechanisms of development of this pathology, many issues of its prevention and therapy have not yet been resolved.
Glandular endometrial hyperplasia - what is it?
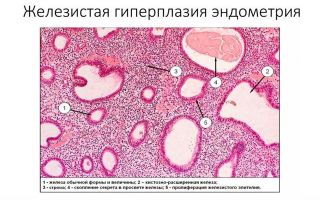
It is one of the main forms of pathological benign changes of a proliferative nature, characterized by proliferation, mainly, of the glandular component of the endometrium and, to a lesser extent, of its stroma, which is accompanied by thickening and increase in volume of the uterine mucosa.
Proliferation is an active process of cell proliferation and can be physiological (cyclical changes in the uterine mucosa) and pathological in nature.
It is this pathological condition that is called “glandular hyperplasia of the endometrium of the proliferative type,” which is dangerous not so much for its widespread prevalence as for its ability to transform into malignant neoplasms of the organ.
The most significant cause of the development of the pathological process is considered to be disturbances in hormonal regulation and feedback in the hypothalamic-pituitary-ovarian system, resulting in a relative or absolute excess of estrogen in the body. These hormonal disorders are accompanied by the absence or insufficient antiestrogenic effect of progesterone.
However, not only hyperestrogenemia is the cause of hyperplastic growths. Molecular biology, clinical immunology, and medical genetics have expanded our understanding of cellular interactions and processes within cells.
It has been established, for example, that not only estrogens, but also cytokines, arachidonic acid metabolic products, growth factors, humoral and cellular immunity systems, an imbalance between cell apoptosis and cell proliferation, disruption of the uterine receptor apparatus, etc. are involved in the regulation of cell proliferation.
So, the main risk factors that determine the development of the pathological process are:
- early appearance of the first menstrual bleeding and late onset of the menopausal period, absence of childbirth;
- hormonal imbalance in the body as a result of dysfunction of the hypothalamus, gonadtropic function of the pituitary gland, thyroid function or hyperplasia of the adrenal cortex;
- hyperprolactinemia, psycho-emotional stress conditions, fasting, etc., contributing to dysfunction of the hypothalamic-pituitary system;
- lack of ovulation due to persistent or atretic follicles;
- ovarian tumors that produce estrogens - theca cell and granulosa cell tumors, stromal hyperplasia, etc.;
- immune disorders, chronic infectious and inflammatory processes of the internal genital organs, repeated abortions and diagnostic curettages, intrauterine contraceptives, smoking - all this disrupts the tissue reception of the uterine mucosa;
- improper and long-term use of Tamoxifen, estrogenic and antiestrogenic drugs, glucocorticoids;
- hyperlipidemia and obesity, diabetes mellitus, metabolic syndrome, insulin resistance;
- diseases of the liver and digestive tract, including the biliary system, leading to disruption of the metabolism of sex hormones;
- arterial hypertension and antihypertensive drugs, coronary heart disease.
As a rule, not one, but several factors are involved in the development of pathological endometrial hyperplasia.
Clinical and histological diagnosis of glandular hyperplasia
In order to systematize the pathology and universality of terminology, a classification was proposed in 1978 (Topchieva O.I.), which took into account the prevalence of hyperplasia.
In accordance with this, the pathological process was distinguished as diffuse and focal glandular endometrial hyperplasia. The latter usually means polyps. In the International Classification, uterine body polyps and endometrial polyps are identified as a separate form.
Ultrasound
The main method of primary instrumental diagnosis of this pathological condition is transvaginal ultrasound, which makes it possible to determine the heterogeneity of acoustic density, the discrepancy between the thickness of the endometrium and the phases of the menstrual cycle, the heterogeneity of its structure, the presence of small glandular cysts or formations of different sizes.
Diagnostic curettage
At the same time, this method does not allow determining the nature of morphological and structural changes in the mucous membrane and causes significant difficulties in identifying glandular polyps. For these purposes, the method of diagnostic separate curettage of the cervical canal and the uterine cavity is used, followed by a laboratory and morphological study of the scrapings obtained.
Depending on the morphological changes in the International Histological Classification, hyperplasia is distinguished:
- Simple without cellular atypia and with cellular atypia.
- Complex, or complex, also with and without cellular atypia.
Simple glandular endometrial hyperplasia without atypia
Transforms into a malignant formation in 1% of cases.
It is characterized by an enlarged endometrium, the structure of which differs from the normal mucous membrane in the uneven arrangement of glands with a uniform distribution of blood vessels. Some glands are enlarged in the form of cystic formations.
The glands and stroma are active, and the balance of growth is maintained between them. The activity is manifested by a significant number of mitoses in epithelial cells. There is no cellular atypia in this form.
- Complex glandular endometrial hyperplasia
- It is characterized by more significant glandular proliferation and an imbalance of the latter between the glandular and stromal components, a structural disturbance of the shape of the glands and the absence of atypia of cells and their nuclei.
- Atypical glandular endometrial hyperplasia
Simple - the incidence of malignancy of which, without treatment, averages 3-8%, and complex - progresses to cancer in 29%. It has the same characteristics as the corresponding (described above) forms, but with the presence of characteristic signs of cellular atypia, expressed in cellular and nuclear polymorphism.
The last one is:
- improper cell division and their different sizes;
- loss of cell polarity;
- excessive staining of cell nuclei and their increase in size;
- red staining of cytoplasmic granules and enlargement of its vacuoles;
- increasing the nuclear-cytoplasmic ratio.
In addition, the contour of the internal epithelial lining of the gland cavity is uneven, forming internal outgrowths in the form of pads or areas similar to the presence of a “gland in a gland.”
In practice, the most common form of atypical hyperplasia is a complex form, in which a large number of irregularly shaped glands are located tightly to each other without penetrating into the stroma, which distinguishes this form from adenocarcinoma.
Hysteroscopy
Another (quite informative) method is hysteroscopic examination. With its help, the following signs of simple glandular transformation are detected:
- mucosal thickness 15 mm;
- the mouths of the fallopian tubes are free in most cases;
- sharp expression of the vascular pattern;
- uneven surface of the endometrium with the presence of numerous folds of pale pink or (less often) bright red color;
- uniform arrangement of the excretory ducts of the glands.
For glandular cystic hyperplasia:
- endometrial thickness exceeds 15 mm;
- a clearly defined vascular pattern with uneven thickness;
- the surface of the mucous membrane has a folded texture and a bright red color;
- visually in the projection of the endometrial vessels located superficially, a large number of cystically dilated glandular cavities and excretory ducts are determined.
Atypical forms do not have characteristic signs during hysteroscopy. They are similar to ordinary glandular cystic hyperplasia. In severe cases, it is possible to visualize glandular growths in the form of polyps of a grayish or dull yellowish color.
Savelyeva G.M. and other authors identified polypoid glandular hyperplasia of the endometrium as a separate form of pathological condition of the mucous membrane, in which:
- its thickness is less than 15 mm;
- the surface is uneven, covered with cysts, pits and grooves of various sizes;
- The uterine cavity along its entire length is filled with pale pink growths that look like polyps and synechiae (adhesions); bubbles are sometimes visible on the surface of polyp-like formations;
- the vascular pattern is significantly pronounced;
- glandular excretory ducts are not identified;
- changes in the fundus of the uterus and along its posterior wall are more pronounced, and therefore the mouths of the fallopian tubes are difficult to visualize.
During hysteroscopic examination, especially before the onset of menstruation, the polypoid form is difficult to distinguish from the state of the endometrium, which is in the late secretory phase.
For more general information about pathology, read the article “Endometrial hyperplasia.”
Clinical picture and possibility of pregnancy
The main clinical symptoms of pathological changes in the endometrium are bleeding and infertility.
Bleeding may occur after a delay in menstruation, coincide with it, or appear during the intermenstrual period (metrorrhagia).
In the latter case, they may have the character of light bloody discharge. Bleeding during menstruation is usually prolonged (more than 7 days) and heavy (menorrhagia), with blood clots.
In a small number of women, the pathology may be asymptomatic.
Possibility of pregnancy
Pregnancy with glandular endometrial hyperplasia is impossible and undesirable, including artificial in vitro fertilization (IVF).
This is due to the fact that, as a rule, fertilization does not occur due to ovulation disorders.
In some cases, when ovulation does occur and the egg is fertilized, pathological disorders in the uterine mucosa prevent its implantation.
Even if pregnancy does occur, especially with a focal form of hyperplasia, its outcome is usually unfavorable - possible termination of pregnancy in the early stages or the formation of congenital developmental defects in the fetus.
In addition, pregnancy in the presence of benign uterine tumors can lead to their rapid growth and malignant transformation (due to a sharp change in hormonal levels).
For these reasons, pregnancy is recommended only after the necessary therapy has been completed.
Treatment of glandular endometrial hyperplasia
Treatment is a rather complex problem. The choice of tactics and methods is carried out taking into account the age and period of a woman’s life, clinical symptoms and the form of pathological changes, the presence of concomitant diseases, metabolic syndrome and insulin resistance, contraindications to the use of certain drugs and their tolerability, etc.
The principles of treatment are:
- Stopping bleeding and prescribing medications that help the body restore blood loss, regardless of age.
- Restoration of the menstrual cycle during reproductive age or acceleration of atrophic changes in the mucous membrane in the perimenopausal period.
- Prevention of relapse.
During adolescence
Oxytocin or Methylergometrine (for uterine contractions), Vikasol, Dicynone, Aminocaproic acid, a complex of vitamins in combination with microelements, and iron-containing agents are prescribed as hemostatic and restorative therapy.
If necessary, hormonal bleeding is stopped using drugs such as Marvelon, Rigevidon, Femoden (until the bleeding stops). If these methods are ineffective, therapeutic and diagnostic curettage is performed.
In order to stop bleeding and contraction of the uterus, you can use treatment with folk remedies, including nettle decoction, extracts of peony, burdock root, mantle and others. However, medicinal herbs do not have any therapeutic effect directly on pathological changes in the endometrium and the causes that caused them.
During reproductive age
After a hysteroscopic examination, separate curettage (for therapeutic and diagnostic purposes) with further histological examination in the absence of atypical cells, hormonal treatment is prescribed - Norethisterone, Dydrogesterone, Medroxyprogesterone, oral combined contraceptive drugs. In the presence of cellular atypia, Diferelin, Buserelin, Danazol, etc. are used.
If the therapy is ineffective or if relapses of atypical or polypoid forms of glandular hyperplasia occur, surgical treatment methods are recommended - resection of the ovaries in case of polycystic disease, removal of the appendages in the presence of hormone-producing ovarian tumors or hysterectomy.
During menopause
At the initial stage of treatment, a hysteroscopic examination with separate curettage is also performed. Depending on the results of the histological examination and if the woman is interested in maintaining the menstrual cycle, hormonal drugs are prescribed according to the appropriate regimens. The duration of taking medications is determined individually.
If there are contraindications to hormonal therapy, as well as in the event of relapses of non-atypical forms of endometrial hyperplasia, surgical hysteroscopic endometrial ablation is possible. The combination of relapses with internal endometriosis or fibroids is an indication for hysterectomy.
During the postmenopausal period
Hormonal therapy is possible in cases of newly diagnosed glandular hyperplasia. In the presence of hormone-producing tumors or relapses, as well as when cellular atypia is established, extirpation of the uterus along with the appendages is recommended.
Thus, pathological glandular proliferation is a complex biological process in which many parts of the regulation of the body’s activities are involved, especially the endocrine, nervous, immune, and digestive systems.
The solution to the question of how to treat this pathological condition and how to prevent its transformation into a malignant tumor largely depends on establishing the nature of the pathological condition of the endometrium and the doctor’s correct understanding of the causative and provoking factors in each individual case.
Source: https://ginekolog-i-ya.ru/zhelezistaya-giperplaziya-endometriya.html
Glandular hyperplasia of the endometrium
Glandular endometrial hyperplasia is a pathology in which the anatomical structure of the tissue of the inner layer of the uterus is disrupted. This disorder consists of excessive growth of glandular cells, as a result of which the endometrial tissue itself increases in volume.
The content of the article:
In general, cyclical changes in endometrial tissue are normal. Cells grow over a period of time under hormonal regulation. The growth process ends with the onset of menstruation and the rejection of excess cells. In this case we are talking about natural hyperplasia.
However, if the glandular layer begins to grow spontaneously (that is, outside the cycle and without the influence of hormones), then we can confidently talk about a disorder in the woman’s body.
Such cell proliferation can lead to the impossibility of reproductive function, and in the worst case, develop into cancer.
Classification of endometrial hyperplasia
Glandular hyperplasia of the endometrium is just one of the types of pathological proliferation of cells in the inner layer of the uterus. Other forms are also known:
- glandular cystic hyperplasia;
- adenomatosis;
- endometrial polyps.
Glandular cystic endometrial hyperplasia occurs when proliferating cells take the form of cysts.
Adenomatosis is the proliferation of cells, accompanied by their structural transformation. As a result, polymorphism of cell nuclei and a decrease in stromal components are observed.
Endometrial polyps are a manifestation of focal hyperplasia, in which not only the glandular epithelium grows, but also the integumentary epithelium, as well as the underlying tissues.
There is another classification - based on the presence of atypia (changes in cell structure). The adenomatosis mentioned above would be classified as complex endometrial hyperplasia. Simple glandular hyperplasia of the endometrium, in turn, consists of a quantitative proliferation of cells. Glandular cystic, as a rule, also does not carry atypia.
Causes of development of glandular endometrial hyperplasia
The main factor that provokes an increase in the growth and rate of division of endometrial cells is hormonal imbalance. A similar situation can arise if the female body does not have enough progesterone, and, on the contrary, too much estrogen is produced.
Against this background, women over 45 who are approaching menopause are at risk. In addition, there are frequent cases of diagnosing glandular endometrial hyperplasia in girls during puberty. Patients of both age categories are affected by hormonal changes.
The development of glandular endometrial hyperplasia and some background genital processes can provoke the development. These include:
- endometritis (inflammation of the inner mucous layer of the uterus);
- endometriosis (abnormal growth of endometrial cells);
- uterine fibroids (benign neoplasm);
- PCOS (polycystic ovary syndrome);
- follicle persistence syndrome (continuation of follicle life despite the fact that ovulation has not occurred);
- formation of follicular cysts.
Gynecological surgical interventions, such as abortions or diagnostic curettages, can also cause this deviation. Women who have not given birth, as well as women who have gone through menopause late, are more likely to become victims of glandular endometrial hyperplasia. Abruptly stopping the use of hormonal contraceptives increases the risk of the disease.
It is worth noting other diseases against which glandular endometrial hyperplasia is more likely to develop:
- obesity;
- hyperglycemia (high blood sugar, including diabetes);
- granulosa cell tumors;
- hypertension (high blood pressure);
- mastopathy (benign pathology of the mammary gland);
- thyroid diseases;
- adrenal gland diseases;
- kidney diseases;
- liver diseases.
A large role in this disorder is given to such a condition as hyperestrogenism.
Symptoms of glandular endometrial hyperplasia
The symptoms of this pathology are often confused with manifestations of uterine fibroids. The main symptom of both is spotting or bleeding that is not associated with the onset of menstruation. Heavy bleeding more often plagues young girls, and women in premenopausal age usually experience spotting.
When it comes to menstruation itself, the bleeding becomes too heavy and lasts longer than usual. Active glandular hyperplasia of the endometrium often leads to the development of anemia in the patient due to large blood losses. In some cases, the menstrual cycle itself gets confused: periods can either be absent for a long time or, conversely, be too frequent.
Since glandular endometrial hyperplasia occurs under the influence of hormonal imbalance, the patient may experience a lack of ovulation and, as a result, infertility. In addition, the hyperplastic layer of the uterus becomes an insurmountable obstacle to the egg, even if it has been fertilized.
But even if pregnancy has occurred, hyperplasia (especially focal) in most cases leads to miscarriage. If you have such a disease, even in vitro fertilization will not help you have a child - doctors will not even undertake the procedure with this diagnosis.
Diagnosis of glandular endometrial hyperplasia
It is immediately worth noting that such a diagnosis cannot be made on the basis of a visual examination, so the diagnosis must certainly be histological. Of course, gynecological and ultrasound examinations should not be neglected, but the final word will be with the results of histological analysis.
Initially, the gynecologist can only by touch determine the enlargement of the uterus in size or its compaction. This will be a reason to conduct a more detailed examination.
Using a transvaginal ultrasound, he will assess the thickness of the walls of the uterus, as well as the condition of the endometrium. An abdominal examination in this case will be uninformative.
In addition, the gynecologist, using ultrasound, needs to simultaneously clarify the presence of cysts or signs of PCOS.
To conduct a histological examination, the woman is sent for diagnostic curettage or aspiration biopsy. These procedures are carried out on the eve of the next menstruation. The information content of hysteroscopy exceeds 94 percent.
This diagnostic method is practically painless, does not require observation in a hospital, and in just a few minutes allows you to obtain material that will give an accurate picture of the disease. Analysis results can be ready in 2 days (if sufficient laboratory resources are available) or in 2 weeks.
Treatment of glandular endometrial hyperplasia
If a diagnosis such as glandular endometrial hyperplasia is made, treatment should follow immediately, since this disease is fraught with transition to cancer. If atypia is not detected, then the goal of treatment will be to prevent uterine bleeding and prevent changes in cellular structures. In this case, after undergoing hormone therapy, a woman can even become pregnant.
If the hyperplasia is atypical, the surgical method of treatment is most often used, namely, removal of the uterus. Although, with the development of medicine, it is increasingly possible to carry out organ-preserving therapy, allowing the patient to experience the joy of motherhood in the future.
It is impossible to give an unambiguous treatment regimen - the fight against glandular endometrial hyperplasia is carried out on an individual basis, taking into account the particular history of a particular woman. Hormone therapy may include several means to stop the proliferation of endometrial cells and at the same time adjust the level of estrogen in the body.
For these purposes the following are used:
- progesterone and its synthetic analogues (gestagens);
- combined oral contraceptives;
- gonadotropin releasing hormone agonists.
Surgical methods do not always involve complete removal of the uterus. The following options are possible:
- scraping of the pathological layer;
- cryotherapy on affected areas;
- laser cauterization.
It is worth noting that hormone therapy can, if not prevent, then at least reduce the volume of surgical intervention. At the same time, after surgery, a course of hormonal medications may be required for more effective recovery.
There are also traditional methods for treating glandular endometrial hyperplasia, but in no case can they replace traditional treatment.
Herbal medicine, including tinctures and decoctions for oral administration and douching, can only have a supportive effect and accelerate recovery.
However, if you focus on traditional methods and completely abandon medical ones, you can cause enormous damage to your health. We must not forget about the risk of hyperplasia degenerating into cancer.
Prevention of glandular endometrial hyperplasia
Obviously, to prevent the development of this pathology, you need to carefully monitor your hormonal levels. This means that every woman should listen to the slightest changes in her body. But you shouldn’t postpone a scheduled inspection until the first symptoms of a malfunction appear.
Competent use of hormonal contraceptives and strict adherence to the doctor’s instructions to refuse them will also help avoid such a dangerous outcome.
A lot also depends on the doctor: the correct selection of contraceptives, timely referral for histological examination, careful management of pregnancy - all this helps prevent the appearance of glandular endometrial hyperplasia in the patient.
Source: https://www.mosmedportal.ru/illness/zhelezistaya-giperplaziya-endometriya/
Glandular endometrial hyperplasia: symptoms, diagnosis and treatment * Diana Clinic in St. Petersburg
Glandular hyperplasia of the endometrium is a consequence of activation of proliferative processes (tissue proliferation) of the mucous membrane of the uterine cavity. Hyperplasia has serious pathological consequences, ranging from disruption of a woman’s reproductive function to malignant transformation of cells with the subsequent development of uterine cancer.
COST OF SOME GYNECOLOGIST SERVICES IN OUR CLINIC IN ST. PETERSBURG
It should be understood that the final diagnosis regarding the type of changes in the endometrium is determined only on the basis of laboratory histological analyzes of a tissue sample, therefore, if you see such a diagnosis in question, there is no need to panic.
Features of the disease
Endometrial hyperplasia is the growth of the endometrium (the inner layer of the uterus), which is benign in nature and causes an enlargement and thickening of the layer. This disease can affect only certain areas of the uterine mucosa (focal hyperplasia) or affect the entire area.
With glandular hyperplasia, it is the glandular tissue of the endometrium that grows and increases in volume. The disease can develop in a woman at any age.
This process is benign and degenerates into cancer only in 1% of cases, but treatment of hyperplasia is still necessary, since the consequence of the pathology is uterine bleeding, anemia, and infertility.
Causes of development of glandular endometrial hyperplasia
The key factor stimulating the development of this pathology is all kinds of hormonal changes.
This is especially evident during the period of age-related and physiological changes in hormonal levels: puberty, pregnancy, lactation, menopause, etc.
In this case, glandular endometrial hyperplasia most often develops against the background of an increase in estrogen levels and at the same time a decrease in progesterone.
There are several categories of concomitant pathological processes that also provoke hyperplastic changes in the structure of the endometrium.
- Genital pathological processes – uterine fibroids, endometritis, endometriosis, polycystic ovary syndrome.
- Extragenital pathological processes - this category includes endocrine disorders such as diabetes, obesity, thyroid diseases, etc.
- Surgical interventions - intrauterine gynecological manipulations, abortions, diagnostic curettages, etc.
Why does glandular hyperplasia of the uterus occur in menopausal women?
The main cause of any type of hyperplasia is hormonal imbalance, so this disease is especially common in menopausal patients.
Normally, after ovulation, a woman produces gestagen hormones, which prevent tissue proliferation and prepare the body for the onset of menstruation. If this does not happen, the body continues to produce estrogens, which cause mucosal growth.
In the cramped uterine cavity, glandular cells have nowhere to grow, so they begin to grow “into themselves,” forming deformed convoluted glands with cystic contents (secretion). As a result, the uterine layers thicken and are rejected, the process is accompanied by bleeding. During this period, you can observe blood with clots consisting of immature cells of the inner uterine layer.
Pathology can be provoked by inflammation in the uterus, myomas and fibroids, sudden refusal of hormonal contraception, surgical abortions and curettage, late menopause.
Forms of glandular hyperplasia
There are three main forms:
- Simple, in its foci there are many glands intertwined with each other;
- Cystic, consisting of overgrown glandular tissues and cysts;
- Mixed, combining two types. As a rule, foci of simple hyperplasia form on the walls of the uterus, and cystic hyperplasia forms on the fundus and corners.
All types of glandular hyperplasia may not produce symptoms for a very long time; in these cases, pathology can be detected only by visiting a gynecologist “just in case.”
Symptoms of glandular endometrial hyperplasia
Normally, the mucous membrane lining the uterine cavity can be divided into basal and functional layers. During the development of glandular hyperplasia, this division is erased, and an increase in the number of glandular structures is observed.
In cases where the glands have cystic changes, doctors talk about glandular cystic hyperplasia. Both of these diagnoses are characterized by a relatively positive prognosis, since these transformations of the mucous membrane are most often not accompanied by malignant degeneration.
The main symptoms of this pathology are bleeding that occurs during the intermenstrual period. This bleeding can be either moderate or heavy, accompanied by clots. However, sometimes such bleeding can be cyclical and recurring.
Bloody “spotting” can begin with glandular hyperplasia on any day of the cycle. This happens because not all tissue is rejected completely. The remaining cells continue to grow, again causing bleeding. Constant blood loss depresses a woman, deprives her of strength and leads to depression.
Prevention of the disease consists of periodic preventive gynecological examinations. This will allow early detection and treatment of glandular endometrial hyperplasia.
Is it possible to get pregnant with hyperplasia?
Pregnancy with this pathology is impossible, because in principle there is no normal menstrual cycle. The egg cannot mature and leave the ovary.
Diagnosis of glandular endometrial hyperplasia
Since bleeding is a symptom of many diseases, glandular hyperplasia is determined using ultrasound and biopsy. To obtain tissue samples, diagnostic curettage or vacuum aspiration (suction of the contents) is performed. The resulting aspirate is sent to the laboratory to confirm the diagnosis and exclude uterine cancer. Hyperplasia is diagnosed with an accuracy of 94.5%.
Progress of the examination:
- Identification of pathology begins with collecting a detailed medical history of the patient, including hereditary factors.
- Next, the specialist conducts a gynecological examination and transvaginal ultrasound (with the insertion of a sensor into the vagina).
- Further, if required, hysteroscopy is prescribed, which involves a visual examination of the uterine cavity using a special optical device.
To determine the type of hyperplastic changes and oncogenicity, an aspiration biopsy of the endometrium (taking tissue from the uterus) and curettage are performed. The latter is often combined with hysteroscopy. After performing a histological examination, the doctor prescribes the necessary hormonal therapy.
Is curettage necessary or are there other treatment methods?
Leaving endometrial hyperplasia untreated is extremely dangerous, since the atypical form can develop into endometrial cancer, cause infertility, and provoke chronic anemia, so curettage must be performed if there are indications for this.
The choice of method depends on the number of lesions and their size. With a small lesion, you can do without curettage. A woman is prescribed gestagenic drugs that eliminate hormonal imbalance.
If it is not possible to stop the bleeding using conservative measures, they resort to curettage or vacuum extraction, removing the overgrown mucosa. Stimulating medications restore ovulation.
In menopausal women, gonadotropin-releasing hormone agonists (GnRH agonists) are used. They create a state of artificial menopause in the body.
Removal of the uterus (hysterectomy) is used as a last resort if the risk of cancer is high. This operation is only permissible for women who do not intend to have children.
Indications for medical curettage
Gynecological curettage is the most effective treatment for endometrial hyperplasia.
The following symptoms may indicate the need for therapeutic and diagnostic curettage of the uterine cavity.
- During menstruation, prolonged and excessive bleeding is observed.
- During menopause, a woman experiences bleeding (from the vagina).
- The patient has vaginal bleeding that is not related to menstruation.
In addition, you should contact a gynecologist if you experience symptoms of anemia, that is, fatigue, constant weakness, fainting, dizziness, lack of appetite, and so on.
Treatment: diagnostic endometrial curettage
Separate surgical curettage of the uterine cavity and hysteroscopy is the most effective surgical method for treating endometrial hyperplasia.
By curettage of the uterine cavity, the doctor uses a curette to remove the hyperplastic endometrium; this is done under the visual supervision of a hysteroscope, which ensures the accuracy of the manipulation.
Of course, curettage is performed under anesthesia, which can be general or local.
Carrying out a separate diagnostic curettage allows you to confirm the presumptive diagnosis of “endometrial hyperplasia”, which is made based on the results of tests and gynecological examination.
The scraping, which is taken as a result of diagnostic curettage, is necessarily subjected to histological examination, which makes it possible to accurately determine the type of hyperplasia. The information content of hysteroscopy, which is performed for endometrial hyperplasia, is estimated by doctors to be approximately 94.5%.
Before and after scraping
Preparation for endometrial curettage necessarily includes passing basic tests, which the doctor will call the patient.
For approximately 3-10 days after curettage, the patient may experience slight bleeding; this is completely normal. In addition to bleeding, particles of resected tissue can also come out after surgery; this is normal.
During the postoperative period, a woman should not allow physical and emotional stress, and sexual contacts are not allowed. Also dangerous are factors such as overheating and hypothermia, failure to comply with intimate hygiene rules.
- Diagnostic curettage in most cases is repeated six months after completing the treatment course, this allows us to evaluate the effectiveness of complex therapy for hyperplasia.
- Where to be examined and treated for endometrial hyperplasia in St. Petersburg and how much does diagnostic curettage cost?
- The prices for curettage for endometrial hyperplasia can be found in the price list of the DIANA network of medical centers or checked with a consultant by phone.
- The Diana Medical Center guarantees the safety of diagnosing glandular endometrial hyperplasia, as well as the development and organization of an effective therapeutic strategy that allows you to get rid of hyperplastic changes forever.
Source: https://medcentr-diana-spb.ru/ginekologiya/zhelezistaya-giperplaziya-endometriya-simptomyi-diagnostika-lechenie/