The retina (retina) is the inner membrane of the visual organ, lining the fundus of the eye.
It performs an important function - it receives light and color signals from surrounding objects and converts them into a nerve impulse for further processing and image reproduction. This is a labor-intensive process. Therefore, many groups of cells are concentrated in the retina, each of which performs strictly assigned functions.
The coordinated work of all retina structures requires good nutrition. It is carried out through an abundant blood supply. Rich blood circulation and many small vessels provide a high risk of retinal vascular pathology and serious complications.
Causes of retinal angiopathy
Angiopathy of the fundus vessels reflects vascular complications of a systemic disease of the body. Retinal vascular pathology may be primary. Although this is most likely a case of an unclear ethological factor. This condition is called idiopathic.
Among the possible causes of retinal vascular angiopathy are:
- diabetes;
- arterial hypertension;
- autoimmune inflammatory lesions of blood vessels (systemic vasculitis);
- hypotension of various origins;
- curvature of the spine (mainly cervical);
- vascular atherosclerosis;
- injuries (face, neck, head);
- intracranial hypertension;
- systemic blood diseases;
- infectious diseases in adolescence;
- birth injuries and antenatal developmental anomalies in newborns;
In addition to diseases occurring with or complicated by retinal angiopathy syndrome, there are also risk factors:
- smoking;
- age over 70 years;
- high radiation;
- hereditary and congenital anomalies of vascular development;
- harmful production factors;
- intoxication.
Often vascular changes are the result of exposure to risk factors or a natural pathogenetic process of the underlying disease. Vascular pathology is called background retinal angiopathy.
Risk group
Patients with diabetes mellitus and hypertension are most susceptible to the disease. There is a particularly high risk of developing retinal angiopathy with frequent “jumps” in blood sugar and pressure and lack of control over the course of the disease.
Elderly people who have passed the age of 70 are at risk due to weakening of the elastic properties of vascular tissue, immunity and greater susceptibility to chronic and infectious diseases.
All patients with hypertension, diabetes, atherosclerosis, vasculitis, and blood diseases should undergo an annual preventive examination by an ophthalmologist.
Screening of special groups of the population is important for early diagnosis and detection of vascular pathologies, the possibility of timely treatment, and improving the prognosis of quality of life.
Workers in hot shops and factories and radioactive stations should also undergo an ophthalmological examination.
Classification of retinal angiopathy
The following types of fundus angiopathy are noted:
- diabetic retinopathy;
- hypertensive type;
- hypotonic type;
- Eales disease;
- childhood angiopathy;
- traumatic type;
- angiopathy during pregnancy.
Diabetic angiopathy
A common cause of retinal vascular pathology is diabetes mellitus. Angiopathy is the result of long-term diabetes. Refers to late vascular complications of the disease and threatens permanent visual impairment, blindness and disability.
Diabetes mellitus is a complex and insidious pathology. The disease involves many organs and tissues in the pathological process. One of the targets is the internal lining of blood vessels. A prerequisite for the occurrence of diabetic angiopathy is an elevated blood glucose level.
When there is too much sugar in the blood and it cannot enter the muscle cells, it begins to bind to blood proteins. Sugared proteins promote the release of vasospasm factors. They also increase the aggregation function of platelets, that is, they increase intravascular coagulation.
This leads to the formation of microthrombi. The permeability of the vascular wall increases. Excess glucose is a trigger for the oxidation of fats, proteins and carbohydrates. Through oxidation, the level of free radicals, which are harmful to the endothelium, increases.
Glucose inside the vessels begins to react to form fructose and sorbitol. These substances are deposited in the cells of the inner lining of blood vessels. As a result of the chemical restructuring, edema develops and the walls of the retinal capillaries thicken. Under the influence of an abundance of chemical and structural changes, vascular cells die and capillaries are destroyed.
Erythrocytes are red blood cells, very plastic structures. Their ability to change shape is necessary for penetration into small arterioles and capillaries for complete blood supply to tissues. Hyperglycemia reduces the plastic properties of red blood cells. Which leads to loss of blood circulation in the retina with its subsequent hypoxia.
A new drug for vision treatment was presented at the Skolkovo Innovation Center. The medicine is not commercial and will not be advertised... Read more
A dangerous addition - retinal angioretinopathy develops quickly. In this case, both eyes are susceptible to pathology. Pathomorphological changes lead to fibrous growth on the retina with transition to the optic nerve head and the threat of irreversible vision loss.
Clinically, retinopathy, like diabetes itself, does not manifest itself in any way. Impaired visual acuity appears at an advanced stage of angiopathy and indicates deep functional and organic changes in the retinal area. Therefore, the diagnosis is made based on the detection of diabetes mellitus and ophthalmological examination of the fundus.
Hypertensive angiopathy
The mechanism of increased pressure is due to the excessive formation of vasoconstrictors - substances that cause vasoconstriction. In arterial hypertension, the vascular wall is constantly in spasm. In addition, the current through the narrowed vessels is increased, the blood is thickened. The same thing happens in the retina.
Constant arteriospasm of the retina, thickening of the blood causes the formation of blood clots, increased wall permeability, swelling and decreased oxygen supply. Gradually, the edematous wall of the vessels is replaced by fibrous (scar) tissue, compressing the venous capillaries and venules.
Symptomatic signs are insignificant and can only appear during episodes of increased pressure - fog, “spots”, “glares” before the eyes.
When a patient has a whole bunch of diseases - diabetes mellitus, hypertension, congenital anomaly of vascular development, smoking with many years of experience (which is very common in medical practice), then it is impossible to determine the exact cause of angiopathy. Then they talk about mixed type angiopathy. This means that vascular pathology of the fundus has developed due to the influence of more than one risk factor.
Hypotonic angiopathy
Retinal angiopathy of the hypotonic type develops with low blood pressure. Hypotension is often considered as a normal variant in thin, young people and athletes. However, low blood pressure can also cause some symptoms: weakness, dizziness, paleness and dry skin.
In the retina, small capillaries become thinner, compensatory blood filling of the veins occurs and their expansion occurs. Insufficient pressure leads to slow blood circulation and retinal hypoxia. A compensatory increase in venous blood supply, coupled with slow blood circulation, contributes to venous stagnation, edema and disruption of the integrity of the vascular wall.
Traumatic angiopathy
Develops with injuries (traumatic compression) of the chest, neck, head, face. In most cases, it is caused by a sharp increase in intracranial and local intravascular pressure. Symptoms include a sharp deterioration in vision, possible rupture of arterioles and capillaries with hemorrhage and traumatic retinal detachment.
Juvenile angiopathy
Applies to persons under 30 years of age. Also known as Eales disease. It is characterized by inflammation of the vessels of the fundus of an unknown etiology. Presumably, the pathology is based on autoimmune vascular damage and a connection with systemic diseases (Behcet's disease, Wegener's granulomatosis). This is a rare but dangerous disease.
Distinctive character - retinal veins are affected more often than arteries. Fibrous tissue grows at the site of inflammation, the affected capillaries are weak and unstable, which is manifested by frequent hemorrhages. Complications of the disease include retinal detachment with loss of vision, early development of cataracts and glaucoma.
Retinal angiopathy in children
The causes of retinal angiopathy in children are serious pathologies of internal organs. These include: diabetes mellitus (type 1), kidney disease, rheumatism, scoliosis, tuberculosis, hypertension, hypotension.
Children are more susceptible to injury. Newborns can be included in a separate group of retinopathy and retinal neuroangiopathy. Diseases arise due to congenital abnormalities in the development of the retina and the vascular network of the organ of vision.
Retinal angiopathy in pregnant women
A feature of the vascular physiology of pregnant women is the appearance of the 3rd circle of blood circulation - the mother-fetus system. This leads to an increase in the volume of total circulating blood, thickening and expansion of the diameter of blood vessels.
And the fragile vessels of the retina are very sensitive to changes. Therefore, a mild degree of angiopathy - detection of dilation and some tortuosity of the retinal vessels during fundus examination - does not pose a threat to the mother or child.
But in women with endocrine and cardiovascular diseases, pregnancy can become a trigger for the development of retinal vascular pathology. Angiopathy that occurred earlier will progress faster.
Therefore, pregnant women should be registered with specialized specialists and undergo regular medical examinations. If complications develop (malignant angiopathy, retinal detachment, threat of vision loss), the issue of caesarean section is decided.
Diagnosis of retinal angiopathy
Diagnosis of the disease begins with a thorough interview of the patient. Usually the patient knows what brought him to the ophthalmologist's chair. Therefore, he tells the doctor about chronic diseases and medications taken “right away.” The examination begins with visometry - assessment of visual acuity using special tables. The following instrumental diagnostic techniques:
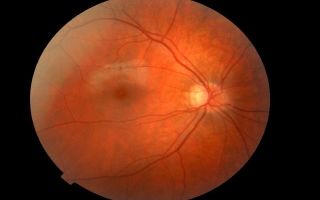
- ophthalmoscopy of the fundus with drug dilation of the pupil - assess the condition of the retina, macula, optic disc, tortuosity, vessel diameter;
- biomicroscopy of the anterior segment of the eye and vitreous body - assessment of the arteries and veins of the eye, the presence of edema, hemorrhage;
- examination of the angle of the anterior chamber of the eye;
- fluorescein angiography of the fundus with the introduction of a contrast agent - allows you to detect early changes in the vessels of the eye;
- optical coherence tomography;
- laboratory tests - as necessary and depending on the underlying disease.
The final diagnosis should include a description of the condition of both eyes, the stage of angiopathy, the presence (if detected) of changes in the central macula, optic nerve head, complications and concomitant diseases of the visual organ.
Example of a final diagnosis: OU – proliferative stage of diabetic retinopathy, grade 3 fibrosis, exudative maculopathy, initial cataract. Diabetes mellitus type 2, moderate, with insulin requirement, uncompensated.
Treatment of retinal angiopathy
The main criterion for therapy control is rational treatment of the underlying disease. This is etiotropic therapy.
Drug therapy
Drug therapy refers to a symptomatic method of treatment, preventing rapid progression and development of complications. Drug groups:
- antiplatelet agents – to thin the blood and prevent the formation of blood clots;
- vitamins B, C, A;
- agents that strengthen the vascular wall and reduce its permeability;
- metabolic drugs.
Laser therapy
A common, fast and painless method of therapy. It also only addresses the superficial problems and does not address the root causes. The essence of laser correction is coagulation (soldering) of “weak” spots on the retina or blood vessels of the eye. All methods of therapy are additions to the treatment of the main systemic pathology.
Complications
Complications develop frequently. The most common is retinal detachment with the threat of irreversible vision loss.
Forecast
If you follow therapy, regularly visit your doctor, maintain a diet and give up bad habits, the prognosis is relatively favorable. It largely depends on the severity of the causative pathology.
Prevention
Specific prevention of retinal angiopathy has not been developed. Prevention methods:
- compliance with doctor's orders;
- regularly attending medical examinations;
- giving up bad habits - alcohol, smoking;
- dieting, proper nutrition, drinking plenty of fluids;
- moderate physical activity – strengthening the muscular framework of blood vessels;
- exclusion of self-administration and withdrawal of medications;
- When playing sports, it is mandatory to wear personal protective equipment for the face and head and adhere to the correct technique.
Source: https://proglazki.ru/bolezni/angiopatiya-setchatki-glaza/
Retinal angiopathy: symptoms, diagnosis, treatment and prevention:
Angiopathy is a lesion, pathology of the vessels of the retina as a result of a disorder of nervous regulation. The result can be either temporary changes or complete blindness.
Symptoms
Retinal angiopathy does not occur immediately. The patient may not notice a decrease in visual acuity for a long period of time and not have any complaints. All changes in blood vessels occur gradually. First, the veins and arteries expand.
Next, changes in their caliber occur, dystonia, paresis, vasospasm, hypoxia of retinal tissue. Visible hemorrhages and branches of the venous bed may appear in the eyeball.
The capillaries become thinner and the overall blood circulation is disrupted.
Causes
Retinal angiopathy most often occurs in people over thirty years of age, but there are cases of the disease in children and adolescents. The etiology of the disease is not clear.
It is believed that the causes of the pathology may be: impaired vascular tone, constant contact with harmful substances, intoxication, hypertension, congenital disorders of the structure of blood vessels, old age, smoking, eye injuries, blood diseases, cervical osteochondrosis.
angiopathy : types
Depending on the causes, the following types of retinal angiopathy are distinguished:
- hypotonic;
- diabetic;
- traumatic;
- hypertensive.
Consequences of this pathology
Retinal angiopathy is dangerous because in complicated cases, one hundred percent loss of vision is sometimes observed. In addition, the disease may result in: partial loss, atrophy or narrowing of the field of vision.
Diagnostics
Only an eye doctor using special equipment can correctly diagnose the pathology. All patient complaints are taken into account.
If necessary, ultrasound, X-ray examinations, Doppler and duplex scanning of blood vessels, and magnetic resonance imaging are performed.
As a result of computer diagnostics, retinal angiopathy of both eyes can be detected.
Treatment
It depends on the type of disease and the presence of complications. Retinal angiopathy is not an independent pathology, so you should look for the root cause of the lesion. In the initial stage, the emphasis is on restoring the microcirculation of the blood vessels of the eyeball and retina. If the cause of the disease is diabetes mellitus, then a diet with limited carbohydrates and dosed physical activity are prescribed to burn excess sugar with muscle mass. Hypertensive angiopathy is treated by normalizing blood pressure and blood cholesterol levels. A cardiologist and a therapist are involved in monitoring the patient. Physiotherapy procedures that are quite effective are: laser irradiation, magnetic therapy, and acupuncture. In severe cases, blood purification – hemodialysis – may be required.
Prevention
It is recommended to reduce the amount of quickly digestible carbohydrates - sweets, cookies, sugar, chocolate, etc. Excessive alcohol consumption causes irreparable damage to health. It is necessary to take control of your emotions, stop smoking, pay special attention to treatment, and lead a healthy and sober lifestyle.
Source: https://www.syl.ru/article/86871/angiopatiya-setchatki-simptomyi-diagnostika-lechenie-i-profilaktika
Retinal angiopathy: what it is, types and symptoms, causes, treatment and consequences
- Retinal angiopathy is a pathological disorder of vascular tone in the fundus of the eye, with disruption of the inflow or outflow of blood, the development of an ischemic process and a gradual decrease in visual acuity.
- Over time, dangerous disabling complications are possible, including rapid blindness, which medicine cannot eliminate.
- The clinical picture is absent or so poor that it cannot be noticed until it is too late.
- In addition, the signs are nonspecific, which makes the disease even more difficult in terms of early diagnosis.
Retinal angiopathy is extremely rarely primary; it is almost always associated with other diagnoses.
Hypertension and diabetes are especially common.
Treatment is conservative. It is possible to radically influence the situation only at the early, first stage. This is an incentive to visit the ophthalmologist more often.
Development mechanism
There is no single way to form a pathological process. The disease does not occur spontaneously, it is the result of a long-term negative influence. Usually internal. We can talk about several ways in which a violation can occur.
- Mechanical factor. Extremely rare. It is based on compression of the fundus arteries. Since the visual organs are relatively well protected, this is unlikely.
Possible immediate causes include helminthic infestations (opisthorchises often penetrate the eyes and enter the body with thermally untreated river fish); tumors are more often observed.
Both pathological processes quickly end in retinal detachment and complete blindness.
An increase in intracranial pressure is somewhat less dangerous. This is a mechanical factor, with it the amount of cerebrospinal fluid increases.
- Excessive load on blood vessels. It occurs much more often. This is almost the main mechanism. Hypertension or a symptomatic increase in blood pressure provokes reflex stenosis (narrowing) of blood vessels.
The reason is biochemical disorders in the system of aldosterone, renin, angiotensin-2. Uncontrolled hypertension provokes chronic angiopathy, which can no longer be treated.
But there is still a chance for correction. Dystrophic processes develop quite quickly on the periphery of the retina.
The fabric becomes thinner and becomes fragile. This is an increased risk factor for detachment and disability.
- Retinal vascular angiopathy is also possible as a result of an anatomical defect. Against the background of diabetes mellitus, an expansion of the third-party network of blood vessels is observed. A reflex narrowing of normal arteries occurs.
In addition, as a result of hormonal imbalance and metabolic dysfunction, there is increased fragility of the blood supply structures. Hence fragility, huge risks of violating the integrity of blood vessels.
The result is a massive release of liquid tissue into the vitreous body. When this structure is filled to at least a third of its volume with blood, retinal detachment is almost inevitable.
A combination of several pathogenetic factors is possible. Then the probability of cure is much lower, and there are much more problems with choosing recovery tactics.
Types and symptoms
Several types of this pathological process can be distinguished. They are the most widespread.
Diabetic angiopathy
- It is in “honorable” second place in the number of cases recorded by ophthalmologists.
- Accompanied by pronounced and fairly rapid pathological changes in the fundus.
- Without therapy, blindness cannot be avoided over the course of several years from decompensation.
Disruption of the normal functioning of the arteries is part of the so-called diabetic retinopathy.
This condition is observed in almost half of patients.
Possible symptoms include:
- Decreased visual acuity. Gradual, for no apparent reason. On one eye or on both sides at once. Depends on the severity of the pathological process.
- Fog in sight. Patients try to rub their eyes, but this makes little sense. The violation goes away on its own after a few seconds from the start.
- Rapid fatigue of the organs of vision, redness of the sclera. Burning and feeling of dryness.
Otherwise, the patient does not feel anything strange. In its development, diabetic angiopathy goes through three stages.
- Non-proliferative lasts the longest. Sometimes for years. And it gives a minimum of discomfort. There may also be no symptoms at all.
- The second stage is accompanied by a violation of the venous-lymphatic outflow, the clinical picture worsens.
- The proliferative stage is associated with the development of a new capillary network on the retina. But these vessels are initially defective and fragile.
The likelihood of them breaking is extremely high. At this stage, the signs are difficult to miss. Often the condition ends in complete blindness.
The process in 80% of cases is characterized from the very beginning as retinal angiopathy of both eyes; unilateral damage is rare.
Attention:
Among all forms of the disease, this one is especially dangerous and aggressive. Requires immediate treatment.
A priori, it is believed that all diabetics suffer from angiopathy; the diagnosis is the basis for examination by an ophthalmologist every 3-6 months.
This seemingly unreasonable expansion of the patient population, overdiagnosis, is indispensable in preserving vision. Because this approach allows you to identify the problem in time.
Hypertensive angiopathy
It develops more sluggishly and slowly. The most common, but less dangerous, because the patient and doctors have more time to select therapeutic tactics.
But this is a dangerous condition; one cannot be mistaken about it. It goes through 4 stages, the clinic is approximately identical throughout the entire pathological process.
Among the signs that exist in all phases of hypertensive type angiopathy:
- Decreased visual acuity. On one or both sides. Asymmetry is considered possible, but it can also be an indication of progressive thrombosis, which is almost guaranteed to lead to blindness.
- Fog in sight.
- Rapid eye fatigue.
- Tearing.
- Problems with concentrating your gaze on one point.
- Double vision, inability to fixate.
Symptoms progress gradually. Starting from the second stage, more specific moments are observed:
- Flickering of flies in the perceived area.
- The formation of black impenetrable spots that interfere with the normal assessment of the image. So-called scotomas. They also occur in other diseases. Rapid differential diagnosis is required.
- Also an increase in the number of floating opacities (they look like transparent and grayish threads, worms, tufts).
Hypertensive retinal angiopathy occurs in 90% of patients at stage 2 of the disease and in 100% of patients with stage 3 hypertension.
Congenital form
Develops in children born prematurely. Accompanied by underdevelopment of the retinal vascular system.
Attention:
This condition can lead to blindness if specific treatment is not started quickly.
Recovery is possible, but in later life the disorder may make itself felt.
Specific symptoms are difficult to determine because the patient is not able to talk about them. Presumably, we are talking about visual impairment of varying severity.
Juvenile type
An extremely rare form of the pathological process. Occurs in only 0.3-0.5% of all patients aged 12 to 19 years.
Accompanied by a sharp arteriospasm (narrowing of blood vessels) without an understandable provoking factor.
In approximately 60% of situations, the first episode ends with hemorrhage into the vitreous body - hemophthalmos. This condition requires urgent help.
Vitrectomy and fluid pumping are performed. Otherwise, blindness cannot be avoided.
Over the next period of time, repeated relapses are likely, so urgent complex treatment is needed under the supervision of an ophthalmologist.
The reasons for the development of such an aggressive process are not precisely known. It is assumed that the provocateur is a hormonal imbalance.
The sex ratio is approximately equal in terms of incidence. Therefore, other reasons are possible.
Hypotonic form
Paradoxically, not only high blood pressure can be to blame for angiopathy. Decreased too.
If in the first case the provocateur is a change in the ratio of specific hormones, too much stress on the vessels, in this case there is poor blood circulation due to insufficient tension in the arteries.
Low blood pressure itself causes angiopathy relatively late. The hypotonic form usually occurs with less severity when compared with its other types.
Symptoms are limited to a slight decrease in visual acuity.
As the disease progresses, the condition of the eyes also worsens. This is a natural process.
Traumatic form
It occurs as a result of physical overload, damage to the head or facial area. The result of this is the destruction of a vessel or several veins/arteries or capillaries at once.
Formally, this is not angiopathy, but rather a complication of injury. But the essence is approximately identical. The most obvious symptoms are: decreased visual acuity, eye pain, fog, double vision, and coordination problems.
The clinic is supplemented by the actual symptoms of the damage received. Some overlap with others, it is important to clearly isolate and differentiate the manifestations.
Basically, in practice, ophthalmologists encounter chronic or background angiopathy, which progresses for many years and does not make itself felt.
But this is only at first glance. Decreased visual acuity, flickering of flies, flashes in the field of view (photopsia), double vision, increased fatigue, burning, stinging, itching, redness. All these are parts of one whole.
Differential diagnosis is necessary to say exactly what is causing this problem.
Causes
Part of the question has already been raised within the framework of the description of the mechanism. If we talk about the direct culprits:
- Hypertension or symptomatic increase in blood pressure. Changes in the fundus are the result of persistent vasoconstriction.
- Defects of the heart, veins, arteries. Systemic circulatory disorders as a result of chromosomal defects. The first time occurs much more often than the second. Genetic abnormalities do not always provoke angiopathy.
- An increase in intracranial pressure due to the influence of cerebrospinal fluid, its excessive amount.
- Hypotension. Low blood pressure readings. The reason is poor blood circulation, and therefore insufficient nutrition of the fundus structures. At the same time, low myocardial contractility is often detected.
In the system, both factors lead to the impossibility of spontaneous independent compensation of the violation.
- Diabetes. One of the record holders for the number of provoked cases.
- Atherosclerotic changes. As a result of smoking, alcohol abuse or excess cholesterol circulation in the blood.
In such a situation, the vessels formally remain the same: there is no narrowing, they are of normal diameter.
In fact, their lumen becomes insufficient: cholesterol clots are deposited on the walls. Plaques.
Over time, this will lead to disastrous results if the patient is not helped.
Risk factors
The more of them, the higher the likelihood of developing angiopathy and the shorter the time frame for the formation of such an alarming outcome:
- Age 65+.
- Occupational hazard. For example, in chemical and weaving industries.
- Unfavorable environmental conditions.
- Pregnancy, peak hormonal states (menstruation, puberty or puberty, menopause).
- Poor diet with lots of fat and salt.
- Smoking. Alcohol consumption. Drug addiction.
Correction of possible risk factors can reduce the likelihood of angiopathy. This is a preventive measure.
Diagnostics
It doesn't present much difficulty. The list of examinations is as follows:
- Interviewing the patient for complaints. In the early stages there are none or the list is meager and vague.
- Anamnesis collection. Lifestyle, habits, especially harmful ones, past and current illnesses. Other factors.
- Ophthalmoscopy with dilated pupil. Standard and contact. Using a Goldmann lens.
The second method is much more informative, since it allows you to examine the far periphery of the fundus. Used as the gold standard for diagnosis.
- Ultrasound. Appointed in controversial cases. Not always required.
- CT. Also not applicable in all situations.
Usually this is enough. If necessary, the list includes a general blood test and a biochemical study (with an extended lipid spectrum, you need to evaluate the cholesterol concentration).
Dopplerography of the vessels of the neck and brain. As part of differential diagnosis.
If there are assumptions about the diabetic nature of the process, a full examination by an endocrinologist is indicated.
Treatment
Therapy is mainly medicinal. Drugs from several pharmaceutical groups are prescribed:
- Means for local restoration of blood circulation in the eyes. Taufon and others.
- Angioprotectors. Reduces vascular fragility. Anavenol, Parmidine.
- Means for correcting the speed of blood movement and circulation: Piracetam, Cavinton.
- Drugs that prevent the formation of blood clots: Aspirin and its analogues for long-term use. Carefully.
Treatment of the underlying disease is also required. Because the above methods do not provide complete recovery. Their function is to protect the eyes themselves.
Antihypertensive drugs are used for high blood pressure. Correction of blood sugar levels as the main method of treating endocrine disorders.
Diabetes also involves vascular coagulation. The essence of the procedure is non-invasive laser cauterization of newly formed capillaries. To avoid hemorrhages. It is painless and safe.
In all cases, non-drug recovery methods are also recommended. Pills alone are not enough.
The measures are simple, although they require willpower:
- Refusal of cigarettes, alcohol and especially drugs.
- Normal sleep of at least 8 hours per night.
- Optimal physical activity.
With retinal dystrophy against the background of angiopathy, not all types of activity are allowed. It is better to clarify the question with an ophthalmologist.
- Proper fortified nutrition. As little animal fat as possible, reducing salt intake (no more than 7 grams per day).
Forecast
At stage 1 - favorable. Because there is every chance of a complete cure. Subject to systemic therapy of the underlying disease and protection of the retina.
At stage 2, it is possible to stop the progression of the disorder and prevent complications.
At stage 3, the prospects are gloomy. It will no longer be possible to slow down the disorder. Therefore, you need to regularly consult an ophthalmologist, especially if risk factors are noted.
Possible consequences
Among the main ones is a decrease in visual acuity. Over time, the vessels become fragile, and the likelihood of their rupture and massive hemorrhage into the vitreous increases. And then retinal detachment cannot be avoided.
This is an emergency condition and requires urgent surgical correction. Without therapy, complete blindness cannot be avoided, without the ability to regain the ability to see.
Finally
Retinal angiopathy is a sluggish, symptomatic, but extremely dangerous disease. Requires constant monitoring and treatment. Without restoration measures it is impossible to achieve lasting results.
The likelihood of complications increases, the most likely of which is loss of eye function. The prognosis is serious, do not neglect the help of an ophthalmologist.
Bibliography:
- EVOLUTION OF CONCEPTS ABOUT HYPERTONIC RETINOPATHY V.S. Zadionchenko, T.V. Adasheva, A.M. Shamshinova, M.A. Arakelyan, Rational Pharmacotherapy in Cardiology 2010;6(6).
- Clinical recommendations. Ophthalmology. Edited by L.K. Moshetova, A.P. Nesterova, E.A. Egorova.
- Federal clinical guidelines for the diagnosis and treatment of diabetic retinopathy and diabetic macular edema.
- Retinopathy of prematurity. Collection of proceedings of a scientific and practical conference with international participation, Moscow, April 6-7, 2016.
Source: https://CardioGid.com/angiopatiya-setchatki/
Retinal angiopathy of both eyes: what is it, symptoms and treatment
Retinal angiopathy is a common ophthalmological pathology in which a change in the structure of the vascular system of the visual apparatus occurs and a disruption of the blood circulation in the eyes.
Retinal capillary angiopathy is observed in many diseases and can lead to serious vision problems.
To detect pathology, ophthalmoscopy and some other instrumental studies are necessary.
Causes
Retinal angiopathy - what is it? This ophthalmological term means a symptom that occurs in various diseases characterized by damage to the circulatory system. This pathological condition is accompanied by changes in the vessels of the fundus, as a result of which the blood supply to the eyes is disrupted and visual functions deteriorate.
The following diseases can provoke the appearance of background angiodystonia of retinal vessels:
- diabetes;
- hypertension;
- atherosclerosis;
- rheumatism;
- thyroid dysfunction;
- autoimmune vasculitis;
- anemia;
- leukemia;
- high intracranial pressure;
- cervical osteochondrosis, scoliosis.
Retinal angiopathy can develop against the background of pathologies of the nervous system, accompanied by dysregulation of vascular tone, as well as congenital heart defects. Among other causes of angiodystonia of the visual organs, the following factors can be identified:
- active smoking;
- overweight;
- work in production with hazardous conditions;
- poisoning of the body;
- individual structural features of vascular walls;
- living in an area with high levels of radiation;
- long-term use of medications that disrupt vascular tone;
- eye injury accompanied by vascular damage;
- genetic predisposition.
Types of angiopathy
Retinal angiopathy occurs as a result of pathological conditions of the body, accompanied by deterioration of blood supply to the fundus of the eye. Such changes in the capillaries of the visual apparatus can appear at any age, but are most often diagnosed in older people. Depending on the nature of the origin, the following types of retinal angiopathy are distinguished:
- Hypertensive. Elevated blood pressure is one of the most common causes of hypertensive angioneuropathy. Arterial hypertension leads to damage to the central artery, narrowing of blood vessels, dilation of veins and damage to retinal tissue. As a result of this, the venous bed branches, pinpoint hemorrhages occur, and the risk of rupture and the development of atherosclerosis increases. With timely treatment of hypertension, the structure of the eye returns to normal.
- Hypotonic. Low blood pressure provokes a slowdown in blood flow and a decrease in the tone of small capillaries, as a result of which the blood thickens and the risk of thrombosis increases. During the diagnostic process, expansion of the arterial network and pulsation of the veins are observed.
- Diabetic. In diabetes mellitus, blood vessels are damaged throughout the body, as a result of which blood circulation is impaired, blood vessels become clogged, the capillary wall swells and vision deteriorates. Due to high levels of glucose in the blood, blood clots form, tissue atrophy begins, and multiple hemorrhages are observed.
Diabetic retinal angiopathy develops in several stages:
- Non-proliferative. Gradual damage to the vessels of the fundus is observed, microscopic aneurysms are formed, and minor hemorrhages develop. This stage is accompanied by swelling of the retina and redness of the iris.
- Preproliferative. Damage occurs to the retinal veins, which become tortuous and dilated. When blood vessels rupture, hemorrhages are observed and venous infiltrates are formed, causing a significant deterioration in vision.
- Proliferative. The most severe degree of diabetic angiopathy, in which new capillaries are formed, characterized by increased fragility. This leads to the appearance of a large number of hemorrhages, causing retinal detachment.
- Traumatic. Due to injuries to the head, neck or eyes, blood vessels are compressed and intracranial pressure increases significantly, which can lead to the formation of leukocyte emboli.
- Youthful. A rare and dangerous form of retinal angiopathy, the nature of which is not precisely known. The pathology develops up to 30 years of age. Juvenile vascular angiodystonia manifests itself through inflammatory processes, hemorrhages and proliferation of connective tissue, which ultimately leads to various complications.
- Congenital. Develops in premature babies due to underdevelopment of the vascular system.
Determining the type of retinal angiopathy is an important point in making a diagnosis, on which the specifics of treatment depend.
Symptoms
The initial stage of development of any form of retinal angiopathy is not accompanied by severe symptoms, which makes timely diagnosis of the problem difficult. Primary signs that may indicate the presence of pathology include:
- blurred visible image;
- flashing “flies” before the eyes;
- short-term darkening;
- deterioration of near visual acuity.
As the disease progresses, the patient may complain of the following symptoms:
- pulsation in the eye area;
- frequent migraines;
- ophthalmotonus;
- pain, pain in the eyes;
- nosebleeds;
- light flickering;
- narrowing of the field of view.
Symptomatic manifestations may differ depending on the type of angiopathy.
The most common form is the hypertensive form, in which there is increased arterial and intraocular pressure, hemorrhages in the retina, and tortuosity of the arteries.
Diabetic angioneuropathy causes redness of the iris, swelling and degeneration of the retina, as well as elevated blood glucose levels.
Diagnostics
If signs of retinal angiopathy appear, you must contact an ophthalmologist, who will make the correct diagnosis and prescribe treatment. To detect a problem, the doctor conducts a detailed survey and examination, after which he prescribes various diagnostic measures. Hypertensive vascular angioneuropathy can be diagnosed using the following studies:
- ophthalmoscopy (examination of the fundus of the eye);
- Vascular ultrasound;
- tonometry (measurement of intraocular pressure);
- visometry (assessment of visual acuity);
- angiography (assessment of vascular patency);
- computer perimetry (study of peripheral parts).
Additionally, there may be a need for CT, MRI, OCT or other instrumental studies.
Retinal angiopathy in children
Hypertensive angiodystonia of the retinal vessels in newborns is a consequence of complicated childbirth, birth trauma, or disturbances in the intrauterine development of the child.
The following factors can provoke the appearance of pathology in a baby:
- poor maternal nutrition during pregnancy;
- genetic predisposition;
- congenital malformations of the cardiovascular system;
- fetal hypoxia;
- premature birth;
- damage to the cervical spine during childbirth.
With proper treatment, retinal angiopathy in newborns goes away within a couple of months. If the baby shows signs of angioneuropathy, then he needs to be shown to a specialist, since this phenomenon may indicate the development of such pathologies:
- diabetes;
- glomerulonephritis;
- renal retinopathy;
- blood pressure disorder.
You should immediately consult an ophthalmologist if you experience the following symptoms:
- blurred visible image;
- poor distance visibility;
- nose bleed;
- hematuria;
- Pain in the eyes;
- loss of vision.
Video
Retinal angiopathy in older children can occur against the background of recent infectious diseases, with VSD, as well as due to disturbances in material metabolism or pathologies in the activity of retinal vessels.
During pregnancy
Retinal angiopathy during pregnancy is a common phenomenon that is encountered by both new and experienced mothers in the 2-3 trimester. Most often, the problem occurs during the 9th month of pregnancy.
Vascular angiodystonia during pregnancy is usually a consequence of hypertension, atherosclerosis or diabetes mellitus. As the embryo grows, the blood volume increases, and pressure surges are observed in stressful situations, provoking stretching of the vascular walls.
This can cause serious complications such as vascular thrombosis, hemorrhage, retinal detachment and vision loss.
Hypertensive angiopathy in a pregnant woman has the following characteristic differences:
- periodic narrowing of the arteries due to toxicosis;
- vascular sclerosis;
- circulatory disorders;
- rapid restoration of the visual system after childbirth.
Treatment of retinal angiopathy with medications
Treatment of retinal angiopathy is selected individually, taking into account the form and degree of development of the pathological condition.
The ophthalmologist selects drug treatment, which should primarily be aimed at eliminating the root cause (hypertension, diabetes, etc.).
For hypertensive angiopathy of the retinal vessels, drug therapy is most often prescribed, consisting of the following drug groups:
- Preparations to improve blood circulation: Vazonit, Trental, Solcoseryl.
- Angioprotectors (normalize wall permeability and blood flow even in the smallest capillaries): Tooxevasin, Detralex, Pentoxifylline.
- Glucocorticosteroids (relieve retinal edema): Dexamethasone.
- Eye drops to improve fundus microcirculation: Taufon, Emoxipin, Quinax.
- Drugs that prevent the formation of blood clots: Curantil, Aspirin, Tiklid.
- Preparations for strengthening vascular walls: Enalapril, Calcium Dobesilate, Prestarium.
- Injections that inhibit the formation of new vessels (prevents hypotrophy of the vascular network): Pegantamib, Bevacizumab.
Additionally, vitamin and mineral complexes are prescribed, including vitamins of groups A, B, C and E. If necessary, other medications are prescribed. For the treatment of retinal angiopathy of the hypertensive type, the following drugs are most often used:
- Parmidine;
- Peritol;
- Emoxipin;
- Lucentis;
- Arbiflex.
Drug therapy for retinal angiopathy is prescribed twice a year. The course of treatment averages 2-3 weeks.
Physiotherapy for angiopathy
The main method of treating retinal angiopathy is drug therapy. To achieve better results and a speedy recovery, doctors often recommend physical therapy. With this diagnosis, the following physiotherapeutic procedures are most often recommended:
- Magnetotherapy. This technique involves exposing the eyes to magnetic field pulses. This helps to dilate blood vessels, relieve swelling and normalize intraocular pressure. Magnetic therapy also accelerates regeneration processes.
- Laser therapy. With the help of periodic low-frequency laser radiation, blood supply to the visual apparatus is improved, inflammatory processes are relieved, and the immune system is strengthened. Laser physiotherapy is not performed during pregnancy, in the presence of oncological processes or pathologies of the nervous system.
- Acupuncture. With the help of special needles, the active points responsible for the state of the visual apparatus are impacted, due to which the microcirculation of the eyes is normalized and visual functions are improved.
- Color therapy. This is one of the best ways to treat hypertensive angiopathy of the retina of both eyes, the essence of which is to influence the nervous system with one color spectrum or another.
At home, for atherosclerotic angiopathy of the retina, it is recommended to use a special physiotherapeutic device - “Sidorenko Glasses”. This device combines several effective physiotherapy procedures that help restore the condition of the visual organs and improve the functioning of the visual apparatus.
Sidorenko glasses can be used even in children starting from the age of three.
Treatment with folk remedies
As a complement to basic therapy, doctors often recommend the use of alternative medicine. For angiopathy of the vessels of the eye, you can use the following folk remedies:
- Well-washed parsley leaves must be chopped using a blender. The resulting mass should be squeezed out through gauze and the remaining juice should be taken orally 2 times a day, 1 tablespoon.
- take 100 grams of birch buds, immortelle, St. John's wort, chamomile and yarrow, mix. Pour a tablespoon of the resulting herbal mixture with 2 cups of boiling water and leave for 20 minutes. You need to add water to the strained broth so that you get 0.5 liters. Take 1 glass in the morning and evening.
- Add 1 tablespoon of cumin seeds and 1 teaspoon of blue cornflower leaves to a glass of boiling water, boil for 5 minutes. Take the resulting decoction 100 ml 2 times a day.
- Add 1 tablespoon of dill seeds to a glass of boiling water, let the product brew for 1 hour, then take 100 ml of the decoction 3 times a day before meals.
To restore vision in case of retinal angiopathy, it is recommended to take tea from currant leaves or rowan fruits. Nutrition plays an important role in the treatment of pathology.
Prevention and prognosis
With timely treatment, hypertensive retinal angiopathy does not pose a threat to vision. However, if the pathological process is started, various complications will begin to develop that can lead to partial or complete loss of vision. You can avoid negative consequences if you consult a doctor on time and follow all his instructions.
The development of angiodystonia and its possible complications can be prevented if the following preventive measures are taken:
- to refuse from bad habits;
- eat properly, balanced;
- maintain eye hygiene;
- avoid excessive visual stress;
- perform visual gymnastics;
- Avoid working in hazardous industries.
Kvasha Anastasia Pavlovna, specialist for the website glazalik.ru
Share your experience and opinion in x.
Source: https://GlazaLik.ru/bolezni-glaz/bolezni-setchatki/angiopatiya/