- September 8, 2018
- Prostate
- Sofia Andreeva
Inflammatory processes in the prostate gland lead to the development of prostatitis. This disease is diagnosed in every third man over the age of 40. It can have an acute or chronic course, provoke complications and significantly worsen the quality of life. One of these negative consequences is prostate sclerosis. Let’s look at what this is in more detail in the article.
Medical certificate
The prostate is an exocrine gland. It has a complex structure of the tubular-alveolar type and performs the most important functions in the body. The health and psychological state of every man depends on the capabilities of the latter.
One of the common pathological disorders that results from inflammatory diseases is prostate sclerosis. According to ICD-10, this disorder has code 42.8.
It is characterized by gradual replacement of muscle and glandular tissues with connective epithelium or scar elements. The structure of the latter is characterized by reduced functional properties.
Therefore, over time, the sexual organ loses its main function - secretion production.
Sclerosis is considered the final stage of inflammatory diseases. Scar changes in tissues are irreversible and lead to damage to adjacent organs (kidneys, bladder, ejaculatory ducts). Pathology is detected in 13% of patients whose medical history previously included a diagnosis of chronic prostatitis.
Main reasons
The replacement of glandular elements with connective tissue is not an independent pathology, but the result of other disorders. Among the main causes of prostate sclerosis, doctors identify the following:
- chronic prostatitis;
- urethro-prostatic reflux;
- vascular atherosclerosis;
- stagnant processes in the pelvis;
- hormonal imbalance;
- surgical interventions;
- age-related changes.
Clinical picture
Symptoms of prostate sclerosis manifest themselves in different ways. The clinical picture is largely determined by anatomical and morphological changes in the gland. However, the following symptoms are common to the disease:
- feeling of incomplete emptying of the bladder;
- frequent and painful urination;
- discomfort in the perineum, groin area and above the pubis;
- sexual dysfunction;
- pain during intimacy.
At the initial stage of the pathological process, symptoms are mild. Most often they resemble an exacerbation of prostatitis. As the disease progresses, the patient is haunted by a constant feeling of thirst and dry mouth, and the condition of the skin worsens. Some develop pyelonephritis and kidney failure.
Types of pathology
Depending on the presence of concomitant diseases, prostate sclerosis is divided into several forms. They differ in specific manifestations. According to the histological classification, which was developed in 1985, the following forms of pathology are distinguished:
- Focal prostatic hyperplasia. The neoplasm is formed from glandular epithelial cells. As a result, the prostate increases significantly in size.
- Parenchyma atrophy. This is a diffuse disorder characterized by depletion of the prostate parenchyma and a decrease in the size of the penis.
- Cystic transformation. Cysts with liquid contents inside form in the gland.
- Nodose adenomatous hyperplasia. Certain areas of the gland begin to grow due to an increase in the number of atypical cells.
In particularly difficult cases, prostate cirrhosis may develop. The pathology is combined with allergic, infectious, interstitial prostatitis.
In addition, all types of sclerotic lesions go through 4 stages in their development. Each of them is characterized by an increase in the manifestation of the underlying disease as it progresses. The change in the severity of symptoms of prostate sclerosis depending on the stage is due to disorders occurring in the body and the involvement of other systems.
The first or initial stage is characterized by impaired functional abilities of the gland and problems with urination. If you consult a doctor in a timely manner, the prognosis is favorable.
The second stage is characterized by malfunctions in the lower and upper urinary canals. At the next stage, urodynamic disorders occur. The fourth stage is considered terminal.
In this case, pathological changes spread to the renal parenchyma, ureters and bladder. The prognosis in most cases is unfavorable.
Diagnostic methods
Timely detection of prostate sclerosis can reduce the likelihood of the disease’s negative impact on other systems and significantly make life easier for the patient. Diagnosis begins with interviewing the patient.
It is important for the doctor to know when the urinary disorder and sexual dysfunction appeared. Separately, he studies the patient’s history and lifestyle.
It is necessary to consider past childhood illnesses and the presence of chronic pathologies.
Then the patient is prescribed a comprehensive diagnosis of the body. It consists of the following activities:
- Urinalysis to detect inflammation in the genitourinary system.
- A blood test to assess the state of the immune system. Determination of the number of erythrocytes and leukocytes. ESR (erythrocyte sedimentation rate) also allows you to determine the inflammatory process in the body.
- A test to detect the level of PSA, prostate-specific antigen, in the blood. Its indicators increase significantly with prostate adenoma or cancer.
- Digital rectal examination to identify the size and density of the gland, the presence of neoplasms.
- Ultrasound of the pelvic organs.
- Transrectal ultrasound to assess the structure of the prostate is carried out using a special sensor that is inserted into the rectum.
- Uroflowmetry, during which the speed of the stream during urination is recorded.
- CT and MRI of the lower abdomen.
- Excretory urography to determine the degree of impairment of urine outflow from the kidneys. The technique involves the use of a contrast agent intravenously. It is eliminated from the body approximately 30 minutes after the procedure.
In some cases, when a patient with prostate sclerosis experiences erectile dysfunction or painful ejaculation, vasovesiculography is prescribed. This examination method allows you to assess the degree of damage to the seminal vesicles.
If an adenoma or cancer is suspected, a biopsy may be required. The study of the material is carried out in laboratory conditions. With its help, a malignant process in the gland is detected.
Treatment Options
Based on a diagnostic examination, the doctor can confirm or refute the preliminary diagnosis of prostate sclerosis. What is it and how long will a person live? These questions are also answered by a specialist during a consultation.
To date, conservative therapy in the treatment of this disease is ineffective. Its help is resorted to in the pre- and postoperative periods to prevent the development of complications. The main method of treatment is surgical or minimally invasive intervention.
Carrying out the operation
Before surgical treatment of prostate sclerosis, the patient must undergo a comprehensive examination of the body. If the following deviations are detected, the operation may be refused:
- last stage of renal failure;
- anemia;
- dementia;
- severe mental disorders;
- any disease in the acute stage.
There are several options for performing the operation. The choice of a specific method of intervention remains with the doctor and depends on the clinical picture and age of the patient.
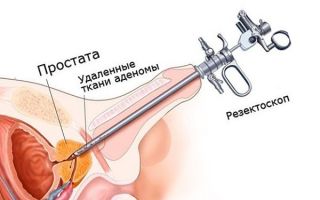
Most often, specialists resort to transurethral resection. This procedure involves excision of sclerotic tissue through the urethra.
It is performed under general anesthesia or using spinal anesthesia. Another treatment method is transvesical prostatectomy.
By making an incision in the bladder mucosa, the doctor makes a circular excision of the pathological areas. The tissue is removed through a transverse urethral incision.
At the initial stages of the disease, transurethral incision is used. The procedure involves installing a tube to remove excrement, which normalizes the flow of urine.
Use of medications
According to doctors, when diagnosed with prostate sclerosis, medication treatment is ineffective. It is not possible to restore scar tissue. Taking medications at the initial stage of development of the disease can only slow down its progression.
However, medications are still prescribed. Properly selected medications help relieve unpleasant symptoms and prevent the growth of pathogenic areas. In the pre- and postoperative periods, medications from the following groups are prescribed:
- Antibiotics (“Summamed”, “Levofloxacin”). Specific antibacterial agents are prescribed based on the type of infectious agent, and broad-spectrum drugs.
- Anti-inflammatory drugs (“Ibuprofen”, “Diclofenac”). Used to relieve and prevent the inflammatory process.
- Vitamin complexes (“Prostate Forte”, “Pro formula”). Prescribed to improve blood microcirculation and boost immunity.
- Alpha adrenergic blockers (Doxazonin, Silodosin). Used to relax the smooth muscles of the bladder, thereby reducing resistance to urine flow.
- Vascular agents (“Curantil”, “Flexital”). Help stimulate peripheral blood circulation, improving the flow in the capillaries supplying the prostate.
All medications, their dosage and duration of administration are selected individually.
Help from traditional medicine
Treatment of prostate sclerosis with folk remedies is ineffective. This method of therapy does not eradicate the disease. On the other hand, it can aggravate the course of the pathological process, causing complications.
However, the use of recipes from traditional healers is permissible during the recovery period after surgery and only in consultation with the doctor. Their main goal in this case is to strengthen the body, weakened by the disease, and normalize the functioning of the genitourinary system.
Due to the obstruction of urine flow, large amounts of toxins accumulate in the body over time. To cleanse the body, folk healers recommend adding watermelon, beets, lingonberries and currants to your daily diet. Decoctions prepared from nettle will also be useful.
There are recipes for strengthening blood vessels and improving blood circulation through the capillaries to the prostate. For example, healers advise drinking pomegranate and birch juices. It is better to alternate drinks. Pomegranate juice should be pre-diluted with water in a 1:1 ratio. You can drink tea with propolis and calendula, or make lingonberry juice. Some patients write in reviews that sage tincture helps.
Prognosis for recovery
If you seek medical help in a timely manner, prostate sclerosis can be cured. However, it is only possible to partially restore the function of the prostate and bladder.
Possible complications
If the patient ignores the initial manifestations of prostate sclerosis and does not rush to seek help from a doctor, the underlying disease can lead to complications. Among them, the most common disorders and disorders are:
- Acute urinary retention, accompanied by a feeling of fullness in the lower abdomen.
- Chronic urinary retention.
- Urolithiasis disease.
- Protrusion of the wall (formation of diverticula) of the bladder.
- Urethrohydronephrosis is an expansion of the ureter and pyelocaliceal system due to prolonged stagnation of urine.
- Vesicoureteral reflux.
- Bacterial inflammation of the kidneys, acute or chronic.
Some patients develop renal failure. This disease is characterized by the inability of the kidneys to remove toxins from the body and maintain proper water-salt balance.
In this case, the patient experiences severe swelling, the volume of urine excreted is reduced, and the pressure increases. In the case of terminal stage of pathology, death is possible. Prostate sclerosis is a serious disease whose treatment should not be neglected.
Only with proper therapy can the occurrence of complications be avoided.
Methods for preventing prostate sclerosis
What kind of illness is this? Is it possible to prevent its occurrence?
First of all, doctors warn that timely diagnosis and concomitant treatment of diseases of the genitourinary system significantly reduces the risk of developing a disorder. In addition, reducing negative factors that directly affect men's health is a kind of prevention. The main measures to prevent the disease are the following:
- undergoing examination by a urologist on a regular basis;
- treatment of pathologies (balanoposthitis, prostatitis, urethritis) immediately after their identification;
- normalization of body weight, fight against excess weight;
- giving up bad habits;
- balanced diet;
- control of motor activity;
- full sexual life;
- compliance with basic rules of personal hygiene;
- use of barrier contraception during sexual intercourse.
According to patient reviews, prostate sclerosis is a complex disease. It is important to identify it promptly and begin treatment immediately. You should not be afraid of surgical intervention, because conservative therapy is powerless in the fight against the disease.
Source:
Prostate sclerosis: symptoms and treatment
Content
Source: https://xn--7-7sbxaakcdcvfl.xn--p1ai/kozha/skleroz-prostaty-simptomy-lechenie-a-takzhe-chto-eto-takoe.html
Prostate sclerosis and its symptoms
Chronic prostatitis is one of the most common diseases among men of reproductive and older age. The disease is an inflammatory process in the prostate gland, which disrupts the process of urination and erection, and also causes pain to the patient.
If a man does not begin to treat prostatitis on time, the disease can provoke many serious complications, for example, the formation of benign hyperplasia, a malignant tumor, complete urinary incontinence, impotence, and prostate sclerosis.
The mechanism of pathology development
Prostate sclerosis is a disease in which the prostate gland degrades. Due to some negative factors, glandular tissue and muscles are replaced by rough connective tissue. As a result, the organ ceases to function normally. The consequences of the pathology manifest themselves in the form of spread of the pathological process to the seminal vesicles and bladder neck.
Depending on the biological processes that occur in the prostate, the disease can manifest itself in various forms:
- Parenchyma atrophy. In this case, the gland atrophies, dries out and decreases in size.
- Hyperplasia. In this case, on the contrary, tissue proliferation and an increase in organ size are observed.
- Cysts in the prostate. Formations filled with liquid are formed.
In more severe cases, it is possible to develop fibrosis of the prostate gland, as well as complete atrophy of the organ.
It is important to note that in addition to the presence of chronic prostatitis, doctors identify a number of factors that stimulate the development of the described pathology:
- allergic reactions;
- weak immunity;
- mechanical injury of the prostate gland;
- vascular pathologies, atherosclerosis;
- hormonal disbalance;
- developmental disorders.
Symptoms of prostate sclerosis
Prostate sclerosis is accompanied by the following symptoms:
- pain in the perineum, lower abdomen, testicles and pelvis as a whole;
- bladder dysfunction, fluid retention;
- frequent urge to urinate;
- renal failure;
- erectile disfunction.
At the beginning of the disease, a sluggish stream is observed, and patients also complain of pain and burning when urinating. If you do not consult a doctor, the sclerotic changes will progress. As a result, the risk of acute urinary retention increases. The patient’s quality of life deteriorates, as he has to get up to go to the toilet several times at night.
Prostate sclerosis almost always leads to deterioration of erection and the development of impotence. Due to testicular damage, the production of testosterone and a man’s libido decreases, and spermatogenesis is disrupted. The consequences of the advanced form of the disease manifest themselves in the form of infertility.
It is important to note that prostate sclerosis does not just disrupt the process of urination, it leads to the reflux of fluid into the kidneys. As a result, inflammation and kidney failure occur, and the likelihood of urolithiasis increases. These conditions are accompanied by renal colic and pain.
Treatment of prostate sclerosis
The disease is accompanied by irreversible changes in the organ, so it is impossible to cure the disease with conservative methods. To diagnose pathology, ultrasound of the prostate, urodynamic study, and urethrocystoscopy are performed.
Ultrasound of the prostate
Treatment of the pathology is surgical - the patient requires removal of the prostate gland. This is necessary in order to restore normal urination and prevent complications on the kidneys. Several years ago, only prostatectomy was performed, which required a large incision in the abdomen.
With the development of endoscopic techniques, removal began to be carried out using a minimally invasive method. This operation is called transurethral resection or TUR; it is performed through the urethra and does not require large incisions and long rehabilitation, like a regular prostatectomy.
Potency problems are a common consequence of organ removal. For such patients, pelvic gymnastics are recommended, and the doctor may also prescribe pills for erectile dysfunction.
Treatment with folk remedies is not carried out, since they are simply not effective in this case. After removal of the gland, the patient can take sedative herbs, but only after consulting with the attending physician.
Conclusion
Prostate sclerosis is a severe complication of chronic prostatitis that cannot be cured with organ-preserving methods. To avoid such a pathology, it is necessary to treat prostatitis in a timely manner, and not to start the disease. And if the problem does appear, you should not refuse treatment, since the pathology will lead to the development of complications for the kidneys.
You might be interested
Source: https://prostatits.ru/oslozhneniya/skleroz-prostaty.html
Prostate sclerosis: treatment and prognosis of the disease
Prostate sclerosis (prostate sclerosis) is a disease that is manifested by compression of the wrinkled parenchyma of the prostate gland of the urethra, narrowing of the vesical sections of the ureters and bladder neck, compression of the seminal flow, resulting in impaired urination, stagnation of urine in the urinary tract, and decreased renal function. and various phases of the copulatory cycle are disrupted. Urologists at the Yusupov Hospital recommend contacting specialists at the first uncomfortable symptoms of the prostate gland, without waiting for the development of sclerotic changes. The clinic’s urologists will prescribe comprehensive treatment that will allow timely treatment of the pathology without the development of complications.
Causes of prostate sclerosis
According to one version of experts, chronic prostatitis leads to the development of prostate sclerosis. In addition, there are suggestions that the etiological role belongs to mechanical effects on the prostate, immunological and allergic factors, developmental abnormalities, vascular atherosclerosis and hormonal effects.
It has been proven that prostate sclerosis is an independent polyetiological disease.
Prostate sclerosis: classification
Since 1985, there has been the following histological classification of prostate sclerosis (according to morphological changes in the prostate, bladder and ureters):
- with focal parenchymal hyperplasia;
- with cystic transformations;
- with nodose adenomatous hyperplasia;
- with parenchymal atrophy.
More severe cases are characterized by the development of prostate cirrhosis, infectious follicular or parenchymal prostatitis, allergic prostatitis, dystrophic and atrophic changes in the prostate.
Prostate sclerosis: diagnosis
When diagnosing prostate sclerosis, the first step is to carefully collect the patient’s life history. The provoking factors for the development of the disease, its clinical manifestations - objective data and the results of studying the functional state of the urinary tract (upper and lower) are studied.
Laboratory tests of urine are carried out: the addition of infection is manifested by the presence of leukocyturia, bacteriuria, erythrocyturia.
The most informative diagnostic method for prostate sclerosis is ultrasound examination of the prostate, bladder, and kidneys.
During the examination, the rate of urination is measured (uroflowmetry), survey and excretory urography, voiding cystourethrography, and electromyography are performed.
To confirm or clarify the diagnosis, a rectal palpation examination of the prostate is prescribed. Sclerosis of the prostate gland is established if it has a dense consistency, reduced size, and pain on palpation.
Prostate sclerosis: treatment
Conservative therapy for prostate sclerosis is used only as an auxiliary method, most often in the pre- and postoperative period.
Some authors consider it advisable to carry out bougienage and catheterization of the urethra. However, these manipulations are not a worthy alternative to surgical treatment, since they are not only ineffective, but can also cause exacerbation of pyelonephritis, urinary tract infection and worsening of the disease.
Surgery is the most effective way to treat sclerosis of pyelonephritis. During surgery, the sclerotic prostate gland is removed and the outflow of urine in the area of the vesicourethral segment is restored.
Prostate sclerosis: surgical treatment
Surgical treatment of the prostate is indicated for patients with the following disorders:
- chronic and acute urinary retention in the presence of increased volume, diverticula, bladder stones;
- disturbances in the outflow of urine from the upper urinary tract in the presence of ureterohydronephrosis, pyelonephritis, vesicoureteral reflux, compensated and latent renal failure;
- urethrovesicular reflux with the presence of empyema of the seminal vesicles.
In addition to the main ones, there are also temporary contraindications to surgical treatment of prostate sclerosis. The operation is not performed for the following problems:
- acute pyelonephritis;
- anemia;
- intermittent stage of chronic renal failure;
Absolute contraindications to surgical treatment of prostate sclerosis are:
- end-stage chronic renal failure;
- senility;
- decompensation of concomitant pathologies;
- psychosis.
Prostate sclerosis: treatment or prevention
The main measure to prevent the development of prostate sclerosis is the treatment of prostatitis. Timely diagnosis of the disease, adequate treatment and adherence to a correct lifestyle helps men control prostatitis and prevent the development of severe consequences that not only cause discomfort, but also pose a threat to their lives.
Modern diagnostics using high-tech equipment are carried out by specialists from the Yusupov Hospital. The clinic cooperates with leading Russian research institutes; in partner clinics, patients receive the most complex treatment methods.
The qualifications of the medical staff, the best diagnostic equipment, the use of the most modern effective treatment regimens for diseases - all this allows us to achieve the best results.
To make an appointment with a clinic specialist, please call.
Tatyana Aleksandrovna Kosova Head of the Department of Rehabilitation Medicine, Physiotherapy Physician, Neurologist, Reflexologist
- ICD-10 (International Classification of Diseases)
- Yusupov Hospital
- Clinical oncourology / Ed. B. P. Matveeva. - M.: ABV-Press, 2011. - 934 p.
- National Guide to Urology / Ed. N. A. Lopatkina. - M.: GEOTAR-Media, 2009. - 1024 p.
- Urolithiasis disease. Modern methods of diagnosis and treatment / Ed. Yu. G. Alyaeva. - M.: GEOTAR-Media, 2010. - 224 p.
*The information on the site is for informational purposes only. All materials and prices posted on the site are not a public offer, defined by the provisions of Art. 437 Civil Code of the Russian Federation. For accurate information, please contact the clinic staff or visit our clinic.
Download price list for services
Source: https://yusupovs.com/articles/neurology/skleroz-predstatelnoy-zhelezy-simptomy-diagnostika-lechenie/
Prostate sclerosis: causes, symptoms, diagnosis, treatment
[block id=”1″]
Like any other disease, prostatitis can have an acute or chronic course, provoke complications and significantly worsen a man’s quality of life.
One of the few complications of prostatitis is prostate sclerosis, which is characterized by pathological thickening of the prostate gland and the replacement of muscle and glandular components with scar tissue.
Such a pathological process ultimately leads to disruption of the functions and structure of the prostate, compression of the bladder neck, urethra and other disorders requiring immediate treatment. These disorders in the male genitourinary system lead to a number of other complications, including impotence and infertility.
Prostate sclerosis is a disease that has a long-term inflammatory process and develops as a result of chronic prostatitis, urotrostatic reflux or against the background of predisposing factors.
In urology, prostate sclerosis can be found under the term “prostate fibrosis.” According to WHO statistics, this disease is diagnosed in 13% of patients with a history of chronic prostatitis.
During the development of the disease, slow pathological changes occur in the prostate gland in the form of wrinkling of the prostate parenchyma and part of the urethra.
In this case, fibrous connective tissues grow, the vas deferens are compressed, the process of urination is disrupted, the functionality of the kidneys is significantly reduced, and urine stagnates in the urinary tract.
Like any other disease, prostate sclerosis has several classifications and stages of development.
Classification of prostate sclerosis
In 1985, a histological classification of prostate sclerosis was developed, which depends on morphological changes in the prostate gland, bladder and ureters.
- focal parenchymal hyperplasia;
- parenchymal atrophy;
- nodose adenomatous hyperplasia;
- cystic transformation.
In more severe cases, cirrhosis of the prostate may develop, which can be combined with infectious follicular or parenchymal prostatitis, allergic prostatitis, or manifest itself in the form of atrophic and dystrophic changes in the prostate gland.
Prostate sclerosis has 4 stages of development:
- Stage 1 – functional changes occur during urination;
- Stage 2 – functional failures appear in the lower and upper urinary canals.
- Stage 3 – characterized by urodynamic disorders, with morphological changes occurring in the organs of the genitourinary system;
- Stage 4 - pathological changes affect the parenchyma of the kidneys, bladder, ureters and seminal canals.
Causes of prostate sclerosis
The main cause of the development of prostate sclerosis is considered to be chronic prostatitis. However, the results of long-term studies have shown that the disease can develop against the background of mechanical, immunological, abnormal and hormonal effects on the human body. So, the main reasons for the development of prostate sclerosis are considered to be:
- chronic prostatitis;
- reflux of urine into the prostate gland through the ducts of the glands during the act of urination;
- stones in the bladder, urethra, prostate gland;
- autoimmune disorders;
- allergic factors;
- exposure to toxic and chemical substances;
- hormonal disorders;
- surgical intervention in the prostate gland;
- atherosclerosis of prostate vessels.
Pathogenesis of prostate sclerosis
In urology, prostate sclerosis is considered the final stage of chronic prostatitis of infectious or non-infectious origin.
During the development of this disease, not only the prostate is damaged, but also the bladder, seminal vesicles, ureter and other tissues of the genitourinary system.
All these disorders can lead to impaired renal function, infertility, impotence and other disorders.
Symptoms of prostate sclerosis
The clinical picture of prostate sclerosis is very diverse and depends on the anatomical and morphological changes in the prostate gland. Prostate sclerosis has characteristic manifestations, which consist of symptoms in which urination is impaired. The following symptoms are characteristic of prostate sclerosis:
- frequent and difficult urination;
- feeling of an unemptied bladder;
- acute urinary retention;
- burning, pain during urination;
- pain in the perineum, above the pubis, groin area and rectum;
- sexual function disorders;
- painful sexual intercourse.
It should be noted that at the beginning of the development of prostate sclerosis, symptoms may be mild and remind the patient of an exacerbation of chronic prostatitis. Every patient with a history of prostate sclerosis has erectile dysfunction.
As the disease progresses and urine outflow is impaired, the patient experiences the following symptoms;
- ureterohydronephrosis;
- chronic pyelonephritis;
- feeling of thirst and dry mouth;
- changes in the skin;
- renal failure.
As a result of the inflammatory process, the prostate gland shrinks, the vas deferens are deformed, stagnant processes develop in the seminal vesicles, and infection occurs.
Prostate sclerosis is the final and irreversible stage of the disease, in which complications develop in the form of vasiculitis, spermatocystitis, and pyelonephritis.
All of the above symptoms may indicate other diseases or disorders, so only a doctor, after the examination results, can make a diagnosis and prescribe appropriate treatment.
Diagnosis of prostate sclerosis
A diagnosis can only be made on the basis of a detailed study of the patient’s medical history, comparing complaints with objective results of urological and laboratory tests. To do this, the doctor conducts a survey and prescribes the following examinations:
- collection of patient complaints - the doctor studies when and how long ago the patient began experiencing difficulties and painful sensations when urinating, or disorders in the sexual sphere;
- collection of life history analysis - medical history and illnesses suffered in childhood are studied. A survey is also conducted - about lifestyle, alcohol consumption, the presence or absence of allergic reactions, chronic diseases of the genitourinary system and the whole body, and other surveys;
- and urine analysis allows the doctor to identify signs of an inflammatory process in the genitourinary system. This analysis determines the number of erythrocytes (red blood cells), leukocytes (white blood cells, immune system cells), also protein, sugar levels in urine, salts, bacteria;
- blood test - determines the presence of an inflammatory process and assesses the state of the immune system. Determines the number of red blood cells, white blood cells, erythrocyte sedimentation rate (ESR);
- biochemical blood test - evaluates the functioning of the liver, kidneys, and pancreas. Shows the amount of blood proteins, fats, microelements;
- Sowing urine on a nutrient medium determines the microbial composition. Allows you to identify the causative agent of the disease;
- Three-glass sample - a triple portion of urine is examined;
- - the first portion of urine - reflects inflammatory processes in the urethra;
- - average portion of urine - reflects bladder diseases;
- - urine examination after prostate massage - reflects the presence and nature of the inflammatory process in the prostate gland.
- Recognize the level of prostate specific antigen in the blood (PSA) - the amount of substances increases in the blood with prostate adenoma, inflammatory processes in the prostate, and prostate cancer;
- Digital rectal examination - performed by a doctor by palpation of the prostate gland. The doctor feels the prostate tissue through the rectum, determines its size, density, presence or absence of nodules;
- Ultrasound examination (ultrasound) of the pelvic organs and kidneys - determines the size, shape, structure of the kidneys;
- Transrectal ultrasound (TRUS) of the prostate gland - determines the volume and structure of the prostate. It is carried out using a special sensor, which is inserted into the rectum;
- Uroflowmetry – the speed of the stream during urination is recorded. This method allows you to identify the degree of disturbances during urination;
- Complex urodynamic study (CUDI) - allows you to determine the functions of the lower urinary tract.
- Computed tomography (CT) of the kidneys and lower abdomen - determines the size of the kidneys, structure, functions and other disorders;
- Excretory urography - allows you to determine the degree of impairment of the outflow of urine from the kidneys. This technique involves the intravenous administration of a contrast agent, which is released from the body 15 to 30 minutes after administration;
- Retrograde cystourethrography - a contrast agent is used, which is injected directly into the urethra and, using x-rays, the shape, structure, abnormalities and presence of narrowings in the urethra are assessed;
- Urethrocystoscopy - the urethra and bladder are examined using a special sensor that is inserted into the urethra. Allows you to evaluate the size and density of the prostate.
In some cases, when the patient experiences a lack of erection, painful ejaculation, and other painful symptoms, then the doctor prescribes vasovesiculography, which allows one to determine the degree of damage to the seminal vesicles. If prostate adenoma or malignant neoplasms in the prostate are suspected, a biopsy is prescribed, which is performed in a laboratory and allows one to determine whether the prostate is benign or malignant.
The results of the above studies allow the doctor to identify the classification and stage of prostate sclerosis, also make the correct diagnosis and prescribe appropriate treatment.
Treatment of prostate sclerosis
The main method of treating prostate sclerosis is surgical. Conservative treatment with the use of drug therapy is carried out only as an auxiliary therapy in the preoperative and postoperative period.
Treatment of prostate sclerosis is aimed at removing the pathological focus, eliminating congestion in the upper urinary tract and restoring the functionality of the bladder and the process of emptying it.
There are several surgical methods that are used for the following symptoms:
- acute urinary retention;
- chronic urinary retention;
- the presence of stones in the bladder or prostate;
- violation of the outflow of urine from the upper urinary tract;
- urethrovesicular reflux;
In addition, there are a number of disorders or diseases for which surgery is not performed or is postponed indefinitely:
- acute pyelonephritis;
- anemia;
- chronic renal failure;
- psychoses;
- senility;
- decompensatory concomitant diseases.
The patient's medical history and examination results will help the doctor conduct and prescribe appropriate treatment. Today, there are several methods of surgical treatment that are used for prostate sclerosis:
- TUR (Transurethral resection) - performed under spinal or general anesthesia. During the operation, a special device with an electric knife in the form of a loop is inserted through the urethra, after which the overgrown tissue is removed, which is sent for histological examination.
- Resection of the prostate gland is performed under general or spinal anesthesia. Scar tissue is removed through the anterior abdominal wall. This method is considered quite traumatic, as it requires opening the bladder and prostate.
- Prostatectomy – scar tissue is removed without affecting the bladder.
- Stent method - the procedure involves widening the urethra tube to improve the flow of urine.
- Epicystostomy – used for the development of acute urinary retention. During the operation, a puncture is made in the abdominal wall above the bladder, after which a tube is inserted into its cavity to drain urine.
These methods of surgical intervention are carried out depending on the patient’s age, stage of the disease and other characteristics of the body.
Complications after treatment
After surgical treatment of prostate sclerosis, the function of the prostate, bladder and kidneys can only be partially restored. In some cases, a number of complications develop in the form of end-stage renal failure, and sometimes death is possible, which is recorded in 2% of patients.
In addition, if treatment is carried out before the development of chronic renal failure, then the prognosis is favorable and the patient has every chance of recovery.
Prevention of prostate sclerosis
It is possible to prevent the development of sclerosis; for this, prostatitis should be treated in time. Timely diagnosis of the disease, quality treatment and a correct lifestyle will help a man keep prostatitis under control and prevent the development of complications that not only cause a lot of discomfort, but also threaten the man’s life.
Source: http://net-prostatita.ru/skleroz-prostaty-prichiny-simptomy-diagnostika-lechenie.html
Prostate sclerosis
- Difficulty urinating (the patient needs to strain the pelvic and abdominal muscles to overcome resistance to the flow of urine).
- Frequent urination.
- Nocturia (night urination)
- Intermittent stream of urine.
- Acute urinary retention (inability to urinate).
- Feeling of incomplete emptying of the bladder.
- Pain in the groin area and rectum.
- Sexual dysfunction (decreased duration and quality of erection (straightening, increase in length and volume of the penis during sexual arousal), dyspareunia (painful sexual intercourse)).
There are several forms of prostate sclerosis.
- Sclerosis of the prostate with focal hyperplasia (the appearance of areas of growth of the gland due to an increase in the number of cells).
- Sclerosis of the prostate with parenchyma atrophy (reduction in the volume of gland tissue due to a decrease in the volume of its cells).
- Prostate sclerosis in combination with nodose (nodular) adenomatous (glandular) hyperplasia (the appearance of areas of gland proliferation due to an increase in the number of cells).
- Sclerosis of the prostate with cystic transformation (the appearance of cysts (cavity formations filled with fluid)).
- Prostate cirrhosis (replacement of gland tissue with connective tissue with disruption of its structure):
- combined with infectious prostatitis (inflammation of the prostate gland);
- combined with allergic prostatitis (inflammation of the prostate gland caused by exposure to allergens);
- without prostatitis.
The main reason for the development of prostate sclerosis is a long-term inflammatory process (prostatitis).
Factors contributing to the development of prostate sclerosis are also considered:
- urethroprostatic reflux (reflux of urine from the urethra into the tubules of the prostate gland), causing sterile (without bacteria) inflammation of the prostate;
- previous operations on the prostate gland;
- the presence of allergic reactions;
- atherosclerosis of the prostate vessels (the appearance in the vessels supplying the prostate gland of atherosclerotic (consisting of cholesterol (a fat-like substance)) plaques that impair blood flow);
- hormonal disorders (lack of testosterone (male sex hormone)).
LookMedBook reminds you that this material is posted for informational purposes only and does not replace medical advice!
-
A urologist will help in treating the disease
Make an appointment with a urologist
- Analysis of complaints (when (how long ago) difficulties and pain when urinating, sexual dysfunction, what the patient associates with the occurrence of these symptoms).
- Filling out a special questionnaire - IPSS: in it you need to answer several questions about the quality of urination, choosing the most suitable options from the proposed ones. Each answer has its own score. The points are then summed up, which allows you to objectively assess the degree of urination disorder.
- Analysis of life history (illnesses suffered in childhood, bad habits, presence of allergic reactions, state of the body’s immune system, chronic diseases of the genitourinary system, sexually transmitted infections).
- Urinalysis - examination of urine for the presence of red blood cells (red blood cells), leukocytes (white blood cells, immune system cells), protein, glucose (blood sugar), bacteria, salts, etc. Allows you to detect signs of inflammation in the organs of the genitourinary system.
- General blood test - counting red blood cells, white blood cells, erythrocyte sedimentation rate - ESR (the time during which red blood cells settle to the bottom of the test tube). Allows you to assess the presence of an inflammatory process and the state of the body's immune system.
- Biochemical blood test (determination of blood proteins, fats, microelements, assessment of liver, kidney, pancreas performance).
- Urine culture (seeding (applying a small amount) of urine to a nutrient medium, coloring it and determining its microbial composition) is used to identify the specific causative agent of the inflammatory process in the urethra and prostate.
- Three-glass sample (triple analysis):
- examination of the first portion of urine (reflects inflammatory processes in the urethra);
- examination of the middle portion of urine (reflects bladder diseases);
- urine examination after prostate massage (reflects the presence and nature of the inflammatory process in the prostate gland).
- Determination of the level of prostate specific antigen in the blood (PSA) - a substance that increases in the blood during benign prostatic hyperplasia (benign neoplasm of the prostate gland), inflammation in the prostate, and prostate cancer (malignant neoplasm of the prostate gland).
- Digital rectal examination - the doctor feels the prostate tissue through the rectum with his finger, determines its size, density, and the presence of nodules.
- Ultrasound examination (ultrasound) of the kidneys and bladder - determination of the size, shape of the kidneys, volume of residual urine after urination.
- Transrectal ultrasound examination (TRUS) of the prostate gland - determination of the volume and structure (density) of the prostate with an ultrasound probe inserted into the rectum.
- Uroflowmetry (registration of urine flow rate during urination). The patient urinates into the toilet, which has sensors installed that estimate the speed and volume of urine per unit of time. The method allows you to identify the degree and type of urination disorder.
- Complex urodynamic study (CUDI) - determination of the function of the lower urinary tract. During the study (using special disposable sensors inserted into the bladder and rectum), the behavior of the bladder during filling and emptying is determined.
- Computed tomography (CT) of the kidneys and abdomen - identifying the size of the kidneys, the condition of their cavity (excretory) system, and ureters.
- Excretory urography (introducing a contrast agent into a vein, taking pictures of the urinary system at different moments of release of the contrast agent, usually 7, 15 and 30 minutes from the moment of drug administration). The method allows you to determine the degree of disturbance of the outflow of urine from the kidneys and the shape of the bladder.
- Retrograde cystourethrography. A substance is injected into the bladder through the urethra, which is visible on an x-ray. The method allows you to evaluate the shape, size of the bladder and the presence of narrowing in the urethra.
- Urethrocystoscopy (examination of the urethra and bladder cavity with a special optical device inserted through the urethra) allows you to visually assess the size and density of the prostate gland.
Treatment of prostate sclerosis is exclusively surgical.
Indications for surgical treatment.
- Acute urinary retention (inability to urinate, accompanied by pain and a feeling of fullness in the lower abdomen).
- Chronic urinary retention (prolonged increase in residual urine volume (the volume of urine remaining in the bladder after urination)) in combination with:
- bladder stone;
- Bladder diverticulum (protrusion of the bladder wall).
- Violation of the outflow of urine from the upper urinary tract (kidneys and ureters), complicated by the development of:
- vesicoureteral reflux (backflow of urine from the bladder into the ureters);
- ureterohydronephrosis (enlargement of the ureter and pyelocaliceal system (the system for storing and excreting urine) of the kidney due to prolonged urinary retention);
- pyelonephritis (kidney inflammation);
- renal failure - the inability of the kidneys to completely remove toxins from the body and maintain a normal water-salt balance: the kidneys are no longer able to produce urine, swelling appears, the amount of urine decreases significantly, and blood pressure rises.
- Urethrovesicular reflux (reflux of urine from the urethra into the seminal vesicles).
Surgical methods of treatment.
- TUR (Transurethral resection): under spinal or general anesthesia, a special device with an electric knife in the form of a loop is inserted through the urethra. The overgrown tissue is cut out, and the resulting tissue is sent for histological examination (studying the structure of the tissue under a microscope).
- Removal of part (resection) of the prostate gland with surgical access through the anterior abdominal wall, while the bladder is either opened or not: a more traumatic procedure, performed under spinal (injection of an anesthetic into the space between the membranes of the spinal cord) or general anesthesia (anesthesia).
- Placement of a tube (stent) at the site of narrowing to improve urine flow.
- If acute urinary retention develops, a tube to drain urine (epicystostomy) is inserted into its cavity through a puncture in the abdomen above the bladder.
- Acute urinary retention (inability to urinate, accompanied by pain and a feeling of fullness in the lower abdomen).
- Chronic urinary retention (prolonged increase in residual urine volume (the volume of urine remaining in the bladder after urination)).
- Formation of stones in the bladder (urolithiasis).
- Formation of diverticula (protrusions of the wall) of the bladder.
- Vesicoureteral reflux (backflow of urine from the bladder into the ureters).
- Ureterohydronephrosis (enlargement of the ureter and pyelocaliceal system (the system for storing and excreting urine) of the kidney due to prolonged urinary retention).
- Acute and chronic pyelonephritis (bacterial inflammation of the kidney).
- Renal failure is the inability of the kidneys to completely remove toxins from the body and maintain a normal water-salt balance: the kidneys are no longer able to produce urine, swelling appears, the amount of urine decreases significantly, and blood pressure increases.
- Timely and sufficient treatment of infectious and inflammatory diseases of the reproductive system:
- Regular visits to a urologist (once a year) for men over 50 years of age.
- Fighting excess weight.
- Active lifestyle.
- Quitting bad habits (smoking, alcohol).
- Compliance with personal hygiene rules.
- Avoid casual sex, use a barrier method of contraception (condom) during sexual intercourse.
Source: https://lookmedbook.ru/disease/skleroz-prostaty