Cervical cancer is a disease that primarily occurs in the anatomical part of the female reproductive organ of the uterus - the cervix. A tumor is the uncontrolled growth of cells in the body, which can be benign or malignant. Treatment may well be successful if the pathology is diagnosed at an early stage and measures are taken in time.
The article was checked by doctor Olga Zorina
Pregnancy and childbirth, Gynecologist, Gynecologist-endocrinologist
Cervical cancer is a malignant pathological mutation of the epithelium located in the cervix.
Cervical cancer according to ICD10: According to the International Classification of Diseases (ICD10), cervical cancer is designated as C53.
Every year, 528 thousand new patients with cervical cancer and 266 thousand deaths from this disease are registered worldwide.
In the structure of mortality from cancer in Russia among women, cervical cancer is 4.8%, which corresponds to 10th place. Mortality in the first year from the moment of diagnosis is 14.6%.
In the age group of 30 - 39 years, mortality from cervical cancer is also maximum (23.6%) compared to other age groups.
Pregnancy and childbirth, Gynecologist, Gynecologist-endocrinologist
Other reasons for doctors’ close attention to the problem:
- latent and practically asymptomatic course of the disease at the initial stage;
- tendency to spread quickly (early metastasis);
- the ability to diagnose the disease at an early stage with timely consultation with a doctor;
- a unique opportunity for effective prevention for the entire group of oncological diseases.
There are no clear causes for this disease, but there are several predisposing risk factors:
- too early sexual life - the epithelium up to 18 years of age has a low protective capacity and is highly susceptible to infection;
- papillomavirus - the development of infection occurs if a woman has a reduced immune system and has a large number of sexual partners;
- genital virus, chlamydia, cytomegalovirus, HIV;
- immune dysfunction due to smoking, obesity, vitamin deficiency;
- decreased local immunity with a complicated obstetric history and taking oral contraceptives.
The problem of identifying signs of cervical cancer in the early stages of the disease is that the symptoms are mild and nonspecific.
Patients may experience:
- periodic small-volume vaginal discharge (leucorrhoea);
- slight occasional itching;
- scant bloody discharge (smears), usually of a contact nature (often after sexual intercourse).
- But all these manifestations can also be observed in other diseases of the genital organs in women.
- To maintain your health and life, it is important to undergo regular preventive examinations with a gynecologist (at least once a year).
- Over the past decade, another predisposing factor has emerged, which is considered the main sign of the possible occurrence of cervical cancer.
In 2008, Dr. Housen was even awarded the Nobel Prize in Medicine for proving the connection between the human papillomavirus and the occurrence of malignant tumors of the cervix. Science has discovered a specific reason for the malfunction of the control system over cell reproduction in the body (see photo).
The mere presence of a virus in the body does not indicate the inevitability of the disease. According to various estimates, the infection rate of the population ranges from 30 to 60%. The main route of transmission is sexual, which explains the widespread spread of the virus. Rare transmission of the virus by contact is possible.
In most cases, the body copes with the pathogen. Only a combination of two factors: existing system damage in the body and the presence of a virus causes tumor growth.
Only viruses with high oncogenicity lead to the development of cancer: 16,18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68, 73, 82 serotypes. Of these, the first three are the most dangerous.
Detection of the causative agent of papillomatosis should be the basis for close observation by a gynecologist and emergency prevention.
Patients come to be examined by a doctor with complaints of:
- the appearance of copious watery vaginal discharge;
- spotting between periods;
- spotting after sexual intercourse;
- bloody discharge from the vagina after defecation (when straining);
- pain in the lower abdomen and pelvic area.
Characteristic of cervical cancer is a tendency to spread rapidly and metastasize. Therefore, as the disease progresses, the symptoms become more and more extensive, adding manifestations of damage to various organs.
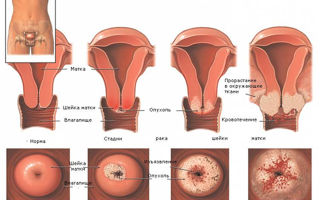
Detection of the disease begins on the gynecological chair during an examination: using a mirror, you can see the unevenness of the edges and color of the cervix. With exophytic cancer (growth towards the vagina), you can see the proliferation of cancer cells; with endophytic cancer (growth towards the uterus), only thickening of the cervix is noticeable.
At the slightest suspicion or for preventive purposes, a specialist performs a smear for oncocytology. The result of the study is to determine the type of cells and confirm or deny malignant changes.
Cervicoscopy, colposcopy and hysteroscopy are methods of hardware examination of the vagina and cervix. In addition to detailed visualization of tissue, these methods make it possible to perform a biopsy of the modified area.
When the question is about the germination of cancer cells into other organs, rectoscopy and cystoscopy are performed. When using ultrasound of the pelvic organs, it is possible to study the size of neoplasms and their characteristics.
The doctor definitely recommends undergoing a number of laboratory tests, including to detect viral infections.
The success of treatment is closely related to the timing of cancer detection. When detected at an early stage, the disease can in most cases be cured, and it is often possible to even preserve the ability to bear children.
The further the process goes, the lower the effectiveness of possible treatment.
If the cancer has not grown beyond the cervix and is located in a small area, the operation is limited to conization of the affected cervix, the appendages and uterus remain intact. In this case, the woman can maintain reproductive function.
If the situation is complicated by a large spread, the uterus is amputated with or without the ovaries. Additionally, lymph node dissection may be performed.
Surgery is combined with chemotherapy or radiation therapy at the doctor's discretion. It has been proven that the combination of these methods with surgery gives a favorable result. Radiation and cytostatic effects can be prescribed before or after surgery.
There are three methods of treating cancer
- surgical;
- radiation therapy;
- chemotherapy.
Surgical exposure
(conization and trachelectomy) consists of surgical removal of a damaged area of tissue or organ (several organs). The problem of effectiveness lies in the relationship between the required radicality of the operation (it is advisable to remove as much of the area as possible to prevent the spread of cancer) with its traumatic impact.
The more the body’s resources are preserved at the time of surgery, the easier and more successful the recovery process after it is. In the later stages of the disease, the method is not used, since the life expectancy of patients after the operation does not exceed the life expectancy without it.
Doctor's advice
Cervical cancer is a tumor leading to loss of reproductive function and disability. It is possible to protect yourself from this disease by regular examination by a gynecologist. Women should not die from diseases of visible localizations!
Radiation therapy
Cell destruction occurs through radiation. Limitations in the use of the method are associated primarily with the degree of prevalence of the malignant process and the volume of affected tissue. The maximum effect is in the middle and early stages.
In the later stages, therapy is not applicable, since the dose required to completely destroy the entire volume of pathological foci exceeds the limit that is safe for the body and becomes destructive.
Chemotherapy
Specific method of influence. It consists of using drugs that are cellular poisons, that is, leading to the death of any cells. The principle of application is based on the fact that actively reproducing cells die faster than others.
The main flaw of the method is the fundamental impossibility of selective action. The impact is not targeted at the source of the disease, but on the entire body. But at the final stages of the disease with widespread metastasis, the use of other methods is impossible, and chemotherapy remains the only available remedy.
- a woman is unable to become pregnant (except for intervention in the form of conization);
- possible inability to have sexual intercourse;
- deterioration of condition due to chemotherapy and radiation therapy;
- hormonal imbalance, if the doctor is forced to remove the ovaries.
Complications in case of refusal of surgery:
- bleeding;
- fistulas between organs;
- thrombosis;
- compression of the ureters with subsequent impairment of renal function.
The life expectancy of a patient in the case of oncological pathology is determined by the severity of the cancer at the time of treatment, its stage and histological identity. You can compare the prognosis by the level of differentiation: for squamous cell carcinoma of the cervix, the prognosis is relatively good, as it is characterized by low mortality.
The sooner the diagnosis is made and treatment instructions are completed, the longer the patient lives.
How long do patients live with stage 1 cervical cancer? How long patients live after surgery is determined by the rate of spread of mutating cells. They begin to extend only beyond the basement membrane, but the size is no more than 4 centimeters. At this stage, the prognosis is as follows: 3/4 of all patients will survive the first five years.
Every second patient has a five-year survival rate if the disease has reached the second stage.
How long do people live with stage 3 cervical cancer: How long people live can only be measured in the next five years. At the third stage, the pressure on the ureters already increases, and atypia spreads in the uterus and vagina. According to statistics, 1/3 of those operated on live more than five years with this stage.
When tumor cells invade the nearby bladder and rectum, survival rate is reduced to 8%.
There is no vaccination against cervical cancer, but since the cause of cervical cancer is the human papillomavirus, in order to prevent the development of cervical cancer, it is advisable for all girls to be vaccinated against HPV before becoming sexually active. There are currently two known cancer vaccines: Gardasil and Cervarix. Vaccination occurs in a course, only three injections over six months.
- Research results indicate persistent protection of the body from cancer transformation; experts speak positively about HPV vaccinations.
- Exchange price - from 5,000 to 15,000 rubles.
- Simple and accessible steps for any woman to prevent the occurrence of the disease:
- careful attention to your condition;
- mandatory regular examination by a gynecologist;
- use of barrier methods of contraception (condoms) to avoid infection with the papillomatosis virus;
- if barrier contraception is not possible, periodic (every six months) infection checks;
- vaccination (a modern vaccine against human papillomavirus has been developed and is available).
Remember that on one side of the scale is the effort, time, money spent, on the other is life.
For information about the causes of the disease and methods of prevention, watch the video:
Source: https://sprosivracha.com/articles/health/96-rak-sheyki-matki-pervye-priznaki-simptomy-na-raznyh-stadiyah-i-lechenie
The first signs of early stage cervical cancer in women
Cancer is a deadly and in most cases incurable disease that manifests itself in the form of a malignant tumor. When cancer develops, the female genital organs are primarily affected - the cervix, mammary glands, ovaries, labia and vagina. The greatest danger to women's health is cervical cancer.
Obvious signs of cancer appear only in the last stages of the disease; women, as a rule, do not pay attention to their presence in the early precancerous period. The intensity and speed of spread of the disease are related to its type. Adenocarcinoma manifests itself most clearly; squamous cell carcinoma of the cervix has fewer symptoms.
Etiology
Before talking about the main signs of cervical cancer, it is necessary to pay a little attention to the etiology of this disease. Thus, thanks to advanced research in this area of medicine, experts were able to prove that the main cause of cancer development in women is human papillomavirus infection.
But naturally, the presence of papillomas on the body is not a reason to panic. Modern scientists have been able to identify more than 100 types of the virus, among which there are also completely harmless strains that provoke the development of easily removable benign formations.
Other possible causes of the appearance of cancer cells in the cervix include:
- genital herpes;
- HIV;
- hidden sexually transmitted infections;
- cervical diseases - erosion, dysplasia and leukoplakia;
- weak immune system;
- abortions, curettage;
- physical abnormalities of the uterus;
- frequent change of sexual partners;
- severe stress.
A direct threat to the female body comes from viruses that infect healthy cells and lead to their degeneration. Diseased cells are transported with lymph to the lymph nodes, which causes the formation of metastases.
Regardless of what caused the cancer, it progresses quite quickly. Unfortunately, with the high rate of spread of the disease, its symptoms remain mild, as mentioned above.
General symptoms
Cervical cancer, unlike a similar tumor in the mammary gland, is quite difficult to detect in a timely manner. Most often, the disease is diagnosed in women between 30 and 55 years old, but under the influence of the etiological factors described above, the disease becomes younger and therefore often occurs in girls younger than 27-25 years old . First of all, girls who have never given birth but have already had an abortion should pay special attention to health, not ignoring even the simplest ailment. The first signs of uterine cancer can hardly be described as specific. Most of the symptoms listed below are easily misleading even to experienced professionals. Thus, when a tumor forms in the cervix of the uterus, which is malignant in nature, a woman experiences:
- Frequent vaginal discharge with an unpleasant color and odor. Typically, vaginal discharge is light, sometimes has a whitish tint, there is no specific odor, and its quantity is minimal. The pathology is copious discharge of a dirty pink or greenish hue that occurs after lifting weights, before menstruation, or after sexual intercourse.
- Papillomas. Warts found on the body do not carry anything good. Their appearance should force a woman to see a doctor. Warts can be the first signal about the presence of a cancerous tumor.
- Pain and bleeding. If your period has not yet arrived, but blood is released from the vagina, then the woman should immediately consult a doctor. It is likely that she began to have uterine bleeding, which requires not only decisive action to stop it, but also to identify the cause of what happened. In some cases, such bleeding occurs after an abortion, miscarriage, during pregnancy, or as a result of excessively active actions during sexual intercourse. If there are no obvious reasons for bleeding, the woman will be sent for examination to identify hidden causes of this pathological condition. A tumor growing on the walls of the uterus leads to drying and cracking of the connective tissue, resulting in pain and bleeding.
- Anemia. Anemia is not typical, but it is still one of the most common signs of cervical cancer. The woman begins to get tired quickly, can no longer cope with the previous volume of housework and job responsibilities, and experiences causeless attacks of suffocation. Anemia can be the result of intrauterine bleeding and a general weakening of the body's immune system that occurs during the development of malignant tumors.
- Constant urge to urinate, sensation of a full bladder. Growing cancer cells lead to an increase in the volume of the uterus, which begins to put pressure on the bladder. The kidneys can no longer cope with such pressure, and the free excretion of urine becomes difficult. With the next urination, only a small part of it is excreted, which causes unpleasant sensations in this area, sometimes pain. Having discovered such symptoms, a woman must contact a urologist, and, if necessary, an oncologist.
- Pain in the back, lower extremities. Under the influence of the tumor, the blood vessels are pinched and the internal organs are compressed. Normal blood circulation is disrupted, which is why most of it does not reach the pelvis and cannot move freely through the vessels. The legs and ankles become swollen and there is severe pain.
- Weight loss. Sudden weight loss never happens without reason. The tumor puts pressure on the internal organs, the intestines cannot cope with the previous volumes of food, appetite disappears, and body weight decreases. Weight loss is always unexpected. If you took strong medications or followed a diet before losing weight, then you probably shouldn’t worry. You should be concerned about an unreasonable loss of 10-20 kilograms of weight in 1-2 months. This practically never happens during normal functioning of the body.
The listed first signs of cervical cancer appear individually.
So, some women lose weight dramatically, but do not experience any obvious discomfort, while others come to the gynecologist with complaints of bleeding and pain after intercourse.
The appearance of any unpleasant and unusual sensations for a healthy body should alert you and force you to consult a doctor. If this is not done, the situation will get out of control and become irreparable.
Adenocarcinoma
The first sign of cervical cancer with adenocarcinoma is pain in the area of the tongue and ears. The digestive tract also reacts to the presence of a tumor. The patient begins to experience sharp, intense pain, dysphagia, and a constant feeling of discomfort. With adenocarcinoma, the following are also observed:
- heartburn;
- loss of appetite;
- anemia;
- pain in the ovaries;
- problems with urination;
- thin, watery white discharge;
- bleeding before menstruation or during menopause.
The reason for contacting a doctor with suspected adenocarcinoma of the cervix may be an unregulated menstrual cycle. The first menstruation in girls usually begins at the age of 12-15 years. After the appearance of the first blood, menstruation may not occur regularly for 2-3 cycles in a row, then the situation stabilizes and the girl can already accurately say when her next menstruation will begin.
The established cycle is interrupted after pregnancy or abortion. In this case, the situation is the same as with the first menstruation. If the menstrual cycle is not due to the reasons indicated above, then the woman should make an appointment for an unscheduled examination with a gynecologist. The cause of the problem is most often a hormonal imbalance, but the possibility of developing cervical cancer should not be ruled out.
Squamous cell carcinoma
The fact that provokes the development of this type of cervical cancer is the human papilloma virus. It occurs in at least 80% of women with a similar diagnosis.
The mucous membrane of the vagina and part of the cervix are covered by stratified squamous non-keratinizing epithelium. A malignant tumor most often occurs at the junction of stratified and columnar epithelium.
The first stage of cervical cancer is not accompanied by any specific symptoms that make it possible to diagnose the squamous cell type of cancer.
Closer to the second and third stages of development, sick women experience:
- heavy bleeding, the development of which is not associated with menstruation;
- the appearance of blood after sexual intercourse (of course, if we are not talking about rupture of the virgin pleura);
- severe pain during sexual intercourse that does not disappear after changing the body position of the partners;
- aching pain in the lower abdomen that has become permanent;
- urinary disturbance;
- constipation
Pronounced clinical signs are observed at the last stage of cancer development; they are usually caused by numerous metastases.
The occurrence of metastases does not allow one to count on a favorable outcome of treatment, therefore, even with extensive experience in stopping bleeding on their own and using painkillers, a woman should consult a doctor.
Only timely diagnosis of the disease will help eliminate the risk of losing your own health and even life.
Stages
The first signs of cervical cancer depend directly on its type and stage, as mentioned above. Experts have identified at least 4 stages of cancer development in this part of the female body:
- Precancerous. Histological examination will show the presence of cancer cells that have not yet had time to penetrate the epithelium. Timely treatment allows you to get rid of not only the symptoms of the disease, but also its cause. Most specialists guarantee a complete recovery.
- Stage 1 cancer. Malignant cells penetrate the epithelium to a depth of 4-5 centimeters, but the tumor is still small and does not extend beyond the cervix. At this stage, possible signs are bleeding from the uterus and severe pain in the lower abdomen.
- Stage 2. The malignant tumor metastasizes and leaves the cervix. The pain intensifies, my back begins to ache, and anemia occurs. The disease at this stage is considered relatively curable.
- Stage 3. The tumor affects the pelvic walls and the upper part of the vagina. The prognosis is unfavorable, the patient loses strength, heavy bleeding occurs, and anemia develops.
- Stage 4. Metastases affect the pelvic organs and lymph nodes, and their active spread throughout the body is observed. The survival rate of women whose disease has reached this stage is low.
Unfortunately, in a number of cases, patients turn to a doctor precisely at the moment the disease moves to stage 4, which suggests a high degree of danger to life from cervical cancer.
The clinical picture at this stage is so unfavorable that nothing can be corrected.
The bleeding practically does not stop, anemia begins, the lower extremities swell, the pain is sharp and does not stop even at night.
Diagnostic methods
Cancer is a terrible diagnosis, so when going to the doctor, many patients unconsciously downplay the extent of their health problems and do not name all the symptoms present. The specialist involved in examining the patient is faced with difficult tasks, and the first place here is occupied by identifying hidden signs of cancer, or those symptoms that the woman does not want to talk about.
So, if a woman turned to a gynecologist, then to determine the causes of her symptoms of illness, the doctor:
- performs a visual examination of the cervix using a special mirror;
- takes a smear for cytological examination;
- uses colcoscopy;
- recommends donating blood for a biopsy;
- refers the patient to a vaginal ultrasound;
- the area of the cervix that aroused his suspicion is visible on the x-ray;
- recommends doing a CT and MRI, and conducting additional laboratory tests.
- If signs of cancer are identified and confirmed, an additional study is performed to assess the level of spread and the number of metastases.
A healthy cervix has a pleasant pink tint, its structure is almost uniform. If there is a malignant formation, an ultrasound machine will show the presence of small ulcers and a change in the color of this organ.
To confirm or refute the preliminary diagnosis, a Schiller test, ultrasound of the kidneys, liver, X-ray of the lungs, examination of the condition of the bladder and rectum, as the organs closest to the uterus, are performed.
Patients are often prescribed intravenous urography, which allows them to determine the functionality of internal organs compressed by a malignant tumor. The main goal of diagnosis is to identify pathology. It is possible that not everything is as bad as it seems to the patient and the doctor himself.
Sometimes test results reveal the most unexpected problems, among which cancer is not even present.
If a malignant tumor is suspected, almost all vital organs are examined. To prevent an identified disease, the symptoms of which a woman did not even suspect, from becoming a cause of severe shock and stress, it is necessary to undergo examination by a gynecologist approximately once every six months.
The disease can be diagnosed immediately upon its appearance and its terrible consequences for the body can be prevented. The risk group for developing cervical cancer includes young women who lead a promiscuous lifestyle, as well as middle-aged women who have reached menopause.
It is important to remember that many diseases get younger over the years. Malignant tumors are no exception, therefore girls should be regularly examined from the moment they enter into first sexual relations.
The unique ability of cancer not to announce its presence for several months and even years is a problem that the best scientists in the world are working to solve.
Video: First signs of cervical cancer in women
Source: https://sheika-matka.ru/rak/pervye-priznaki-raka-shejki-matki-ploskokletochnyj-rak-adenokarcinoma/
Cervical cancer: a preventable disease
Cervical cancer is merciless. More than 500,000 new cases of cervical cancer are registered annually around the world, and about 53% of women die. In our country, this cancer kills 21 women every day. We know a lot about this disease, because the cervix is an organ that is quite accessible to examination. Why are we still diagnosing things too late?
Cervical cancer
A disease with a well-studied and proven cause. In 2008, Harald zur Hausen won the Nobel Prize for proving the connection between HPV infection (human papillomavirus) and the development of cervical cancer.
Back in 1983, he managed to discover the most aggressive type of virus - HPV-16.
Over 34 years of research, which involved more than 10,000 patients, it was proven that 95% of cervical cancer cases are associated with one of the types - HPV-16 or HPV-18.
As always, a new idea captured hearts and minds. Thousands of doctors then rushed to look for HPV in millions of women, followed by monstrous attempts to get rid of the pathogen at any cost. In my memory, dozens of drugs came onto the market with the promise of “cure HPV forever.” Enthusiastic reviews gave way to bewilderment and disappointment.
Each subsequent medicine became more expensive than the previous one, each was accompanied by evidence of effectiveness in the form of studies of varying degrees of homegrown. I can safely say that we have definitely achieved only one effect - we have created HPV hysteria in the space around us.
“HPV cure” has become so popular that I am no longer surprised by claims that someone was cured of HPV with cow pats or Allokin-alpha.
Time for the big scare
Now it is obvious to most specialists: HPV is highly contagious; most sexually active women with more than one partner encounter HPV at least once in their lives. HPV is an epitheliotropic virus.
It lives in the thickness of the epithelial layer on the cervix, vaginal walls or on the skin of the external genitalia.
Moreover, we often see the place of its “registration” through a colposcope, and the results of vital activity in the form of atypical cells end up in cytological smears.
Women who have been diagnosed with HPV often cry in my office. Their last hope is for a “magic pill” that will cure the evil virus. In fact, there is no reason for tears yet.
In most cases, HPV infection does not require any treatment at all, because the virus is spontaneously eliminated - it leaves the body on its own without any treatment along with the exfoliating cells of the stratified squamous epithelium.
If the HPV test is positive, but there are no colposcopic and cytological signs of damage, no treatment is required.
The senseless and merciless use of immunotherapy drugs for the latent form of HPV infection causes damage not only to the wallet, but also, possibly, to the body.
Admittedly, our actions in relation to the immune system are suspiciously reminiscent of the pirouettes of a bull in a china shop.
We can’t even proudly boast: “I cured Ivanova’s latent form of HPV!” Because it is impossible to prove why the virus left the body. Either he did it voluntarily, or he somehow got bored with our medicinal shamanism.
The younger the woman, the higher the likelihood of spontaneous elimination. Most experts consider it inappropriate to routinely test sexually active women under 25 years of age for HPV.
However, these patients with latent forms of HPV require careful monitoring. We will have to repeat the examination once or twice a year to make sure that HPV has left the body.
The average time for self-elimination of the virus is 1.5 years.
If the same type of HPV was detected three times over the course of 1.5–2 years, we can talk about persistence. Persistence can also be suspected if the viral load is high in women over 30 years of age. This in no way means that the patient has cervical cancer or its prestages, but, of course, indicates a significant risk and requires the same thing - careful monitoring.
Persistence of HPV without colposcopic and cytological signs of damage is not a reason for treatment.
And then, like Khoja Nasreddin: either the donkey dies or the sultan dies. Either HPV will leave the body, or we will still “catch” changes in cytology or colposcopy.
Why get tested?
Firstly, in order to identify a favorable group - women without HPV. They can be invited for screening less often (provided they have a monogamous sexual relationship); the risk of developing cervical cancer in this group is minimal.
Already in 2009, it was possible to prove that HPV-negative CIN (pre-stage cervical cancer) is impossible. If the results of a cytological examination indicate a precancerous condition of the cervix, and tests for HPV are negative, then someone is mistaken.
I often offer the mantra to my patients: “No HPV, no cervical cancer.” However, it must be remembered that the human factor has not been canceled.
Errors when taking material for research, errors during storage and transportation, and errors during research can create a picture of false well-being. HPV testing is not the gold standard.
Everything should be assessed in combination with cytology and colposcopy.
Who really needs HPV testing:
- patients with unclear results of cytological smears;
- after surgical treatment of precancerous diseases of the cervix - CIN;
- as a regular screening for patients over 25 years of age;
- with questionable results of colposcopy.
Cervical cancer develops very slowly. From the moment HPV enters the body to the development of cancer, years, and sometimes even decades, pass.
At first, the activity of the virus is almost invisible, but as soon as it is integrated into the genome of the cells, we will see characteristic changes in cytological smears.
Koilocytes ("empty" cells typical of HPV infection) and dikaryosis (various disorders in the cell nucleus, multinucleated cells) appear. This stage can last from 3 to 20 months.
Under unfavorable conditions, real cancer cells appear on the lower layers of the epithelial layer, where the most active cell division occurs. This is CIN I (mild dysplasia or grade 1 cervical intraepithelial neoplasia). As scary as it sounds, CIN I is not cancer; it develops many years before actual cancer.
In stage CIN I, the disease is reversible.
For young women and/or women planning pregnancy, we have the right to continue observation for 1.5 to 2 years. If the process is not going to regress, treatment is carried out.
Drug therapy is ineffective and can be used either as an auxiliary method or not at all.
And treatment is the complete removal of the lesion: excision (removal of the affected area) or conization (removal of a cone-shaped fragment of the cervix).
On average, CIN I turns into CIN II–III in 3–5 years (of course, the process will be much faster with concomitant HIV infection, chlamydia or gonorrhea). But there is still nothing irreparable at these stages. If we “caught” the patient at stages CIN II – CIN III, then wide excision of the affected areas is performed: excision or conization of the cervix.
A young woman with CIN I, having read horror stories on the Internet, sobs bitterly:
- Why are you crying so much? — I read that I will have cancer! I will die! - But you are already here. We would be worthless on a market day if we did not know how to identify and treat this stage.
After all, this is exactly why you came to the gynecologist - so that you don’t miss CIN. We didn't miss it. Now let’s carefully remove everything and continue to observe. - Will I be able to give birth? - Necessarily.
- When will it be possible to get pregnant?
- You can start 6 weeks after surgery.
Wide excision of the affected areas with a loop of a radio wave apparatus is a simple procedure. We mostly do this on an outpatient basis under local anesthesia. The entire removed area is sent for histological examination.
If it's so simple, why are women still dying?
This is a cruel and valid question. Cervical cancer is always someone's fault. Although, of course, if a woman did not go to the gynecologist’s office for 10 years, only doing an ultrasound from time to time, anything could be grown.
Olga was 44 years old. I leafed through her outpatient card: gynecologist, gynecologist, gynecologist... Over the past 10 years, she gave birth to three children and had 4 abortions. There is not a single cytological smear in the card. In the mirrors - advanced cervical cancer, symptomatic treatment.
Elena, 32 years old. She gave birth to 2 children with an interval of 2 years, came for an appointment 4 months after the second birth. Cytological smears were taken twice during pregnancies, but probably very gently for fear of spotting. In the mirrors - cervical cancer, stage IIb - we will be treated.
Marina, 38 years old, cook. He undergoes regular medical examinations and shows his health certificate. In the mirrors - advanced cervical cancer, stage III, we will be treated, but the prognosis is very doubtful. I doubt she was examined in mirrors at all. Perhaps they took smears for gonorrhea and trichomoniasis without looking. The most annoying thing is that Olga was sure that everything was fine with her, since she was regularly examined.
Cervical cancer is a disease of the young. The peak incidence in our country occurs at the age of 30–35 years. The cervix is an easily accessible object for research, which makes each case of advanced cancer even worse. The disease is easily preventable by catching it at the CIN stage. And the woman will get married, and give birth to a child or three, and live a long and colorful life.
My youngest patient with invasive cervical cancer was 23 years old. A young man brought her by the hand to be examined for infection. The young man was bothered by the unpleasant smell of his beloved’s discharge. Wertheim's operation, radiation therapy, then relapse, chemotherapy. She died 2 years after diagnosis.
The human factor cannot be ignored...
Some did not come to the appointment, some did not take a cytological smear or did not collect the material well enough, some did not examine single atypical cells due to pronounced inflammatory changes.
There are many reasons for late diagnosis. It takes years from the introduction of HPV into the genome of epithelial cells to the onset of cancer, but invasive cancer grows and progresses very quickly.
Today, a new cervical screening strategy is being implemented everywhere in the Russian Federation - the use of liquid cytology with HPV testing. This significantly increases the chances of early diagnosis of cancer. It is this problem that gynecologists should deal with, and not “cauterizing erosions” and a merciless battle with HPV.
Let's set goals correctly. We strive to catch cancer in its pre-stages and neutralize it. “Cauterizing” everything that turns red does not help the diagnosis; on the contrary, it creates serious difficulties, masking a slowly smoldering process.
Hunting for CIN
The implementation of a simple algorithm guarantees timely diagnosis of changes in the cervix.
- Smears for oncocytology must be done for all women who are sexually active. You can do it annually, but not less than every 3–5 years. Women over 25 years of age should undergo HPV testing along with cytology.
- A “bad” cytology smear and/or detected HPV requires mandatory colposcopy. An unclear red spot on the cervix, even with “good” cytological smears and the absence of HPV, requires mandatory colposcopy.
- Abnormal colposcopy results require taking a biopsy from all suspicious areas, or, which is more correct and cheaper, performing a wide biopsy of the cervix.
After treatment for CIN, continued follow-up for at least 5 years is strongly recommended. Anything can happen—the disease can recur. If you don't lose sight of it for a couple of years, you can notice a relapse in time and prevent the development of invasive cancer.
Oksana Bogdashevskaya
Photos 1- thinkstockphotos.com, 2-5 - provided by the author
Source: https://apteka.ru/info/articles/zhenskoe-zdorove/rak-sheyki-matki-bolezn-predotvratima/
Symptoms and treatment of cervical cancer
It is difficult to recognize cervical cancer at an early stage, since the clinical symptoms of this oncological pathology are almost completely absent.
That is why such a disease is dangerous and causes severe complications from which a woman can die.
At the initial stage of development and adequately selected therapy, the disease can be cured, otherwise the survival prognosis worsens significantly.
Reasons why cancer occurs
The main factor giving impetus to the progression of such a dangerous disease is infection of the body with human papillomavirus infection. A pathogen that affects the cervical region first leads to the development of dysplasia, but if the pathology is not identified and treated in a timely manner, cancerous degeneration occurs, and oncology develops rapidly.
Other common causes of cervical cancer are:
- hormonal and endocrine disruptions, which most often occur in old age, when a woman enters the menopause phase;
- chronic infectious lesions of the vaginal mucosa, cervix and uterine body;
- injuries received after childbirth, during sexual intercourse or diagnostic examination;
- early onset of sexual activity, a large number of sexual partners, unprotected sex;
- abuse of bad habits;
- unfavorable environmental environment;
- uncontrolled use of oral contraceptives;
- multiple births or frequent terminations of pregnancy.
Obesity is a prerequisite for the development of uterine cancer, so overweight women are at risk.
Risk factors for cancer are:
- decreased protective functions of the body;
- obesity;
- deficiency of vitamins A and C;
- parakeratosis, erosion and dysplasia of the cervix.
Source: https://InfoOnkolog.ru/lokalizatsia/moch-sistema/rak-sheyki-matki.html
Cervical cancer: symptoms and signs
This is an oncological disease in which malignant degeneration of the mucous membrane of the cervix is diagnosed. In terms of the frequency of clinically detected cases, cervical cancer exceeds only breast cancer and endometrial cancer.
The main risk area for developing cervical cancer is women between 40 and 55 years of age. But lately the disease has become catastrophically younger. Increasingly, cervical cancer (cervical cancer) is being diagnosed in patients under 30 years of age.
There is another problem - late diagnosis. Although the disease is fairly easy to detect, in more than half of cases, cervical cancer is found in late stages.
If you suspect a disease, you should immediately consult a gynecologist.
Types of cervical cancer
The main classification of cervical cancer follows from the type of tissue affected by the tumor. The topmost and protective layer is the squamous epithelium. In this case, we can talk about the following forms:
- Dysplasia (it can have 3 degrees) is a precancerous condition;
- Cancer in situ. This is the name given to the degree of tumor with minimal growth into other layers;
- Squamous cell carcinoma of the uterus.
The following types of squamous cell carcinoma of the cervix may manifest themselves:
- Papillary;
- Warty;
- keratinizing;
- Non-keratinizing;
- Lymphoepithelioma-like;
- Basaloid;
- Squamous transitional.
Tumors affecting the secreting epithelium are called adenocarcinomas. They can be:
- Endometrioid;
- Serous;
- Clear cell;
- Mesonephric;
- Mucinous.
The process is often accompanied by the formation of concomitant tumors of other etiologies:
- Neuroendocrine and large cell carcinomas;
- Carcinoids;
- Sarcomas;
- Small cell cervical cancer.
Classification of cancer forms
Cancer is distinguished by location (vaginal part of the cervix and internal part). In addition, there are several forms of growth:
- Pre-invasive. In this case, stage zero is assigned. The malignant process develops strictly within the epithelium;
- Microinvasive. The depth of the lesion does not exceed 0.5 cm, without metastases;
- Non-invasive (stage 1). Cervical cancer cells are not widespread and progress very slowly;
- Exophytic. The most common type, in which the tumor grows in the lumen of the vagina. Externally it resembles cauliflower forks. This is stage 3 (with damage to vaginal tissue). At stage 4, metastases to various organs may be observed;
- Endophytic. The tumor grows secretly in the cervical canal. It becomes noticeable only in the later stages of tumor decay, leading to looseness and unevenness of the cervix. Externally it is defined as a bleeding ulcer that grows deep into the tissues of the uterus;
- Mixed. This is a rather rare option, since it involves the presence of several tumors of different types at once.
Causes
The main threat to cervical cancer in women is viruses, which lead to mutations and the degeneration of healthy tissue cells into malignant formations. The No. 1 risk factor is human papillomavirus (HPV). But this virus has more than 100 varieties with varying degrees of risk of developing cancer. It is because of this feature that over 90% of cases of cervical cancer develop. After entering the body, the HPV virus can occur in 3 forms:
- Asymptomatic form;
- Subclinical form;
- Clinical form. In the genital area there are multiple or single growths (condylomas and papillomas).
The most dangerous and with a high level of oncogenic risk are HPV strains carrying markers 16, 18, 45 and 46. The average level of risk for developing cervical cancer are strains of types 31, 33, 51, 52 and 58.
Other causes of cervical cancer:
- Predisposition. If women have had cases of cervical cancer among their relatives, then they should be extremely careful about their health and undergo regular examinations;
- Viruses - genital herpes, HIV, chlamydia, cytomegalovirus;
- Untreated or incompletely treated genital infections;
- Diseases of the cervix, accompanied by changes in tissue (erosions, dysplasia, leukoplakia);
- The presence of benign tumors (fibroids, fibroids), which under long-term unfavorable conditions can degenerate into malignant and other neoplasms;
- Severe weakening of the immune system;
- Uncontrolled human exposure to radiation, chemical toxins;
- Frequent abortions or curettages, as well as complications associated with these and other surgical procedures;
- Frequently recurring pregnancies and childbirths;
- Microtraumas of the cervix or uterus itself, as well as the cervical canal;
- Early onset of sexual activity;
- Change of partners more often than 2-3 times a year;
- Long-term stress;
- Uncontrolled use of oral combined contraceptives;
- Long-term smoking or addiction to alcohol;
- The presence of chronic inflammation in the pelvic area without proper treatment. Other chronic diseases associated with inflammatory processes.
Symptoms
The main and most alarming symptoms are:
- Unexpected and frequent bleeding (after a visit to the gynecologist, after sexual intercourse, between normal periods, during menopause);
- Menstrual bleeding lasts more than a week;
- Discharge with blood, it may have an unpleasant odor and signal the beginning of tumor decay;
- Purulent discharge with a pungent and unpleasant odor;
- Prolonged pain (lower abdomen and uterine area);
- Pain that is spasmodic in nature. In this case, some of the pain may radiate to the lower back;
- Excessive vaginal dryness and pain during sexual intercourse;
- Sudden weight loss (from 10 to 15 kg in a few weeks). This symptom is unconditional and requires prompt medical attention;
- Constant constipation and pain during bowel movements. Other diseases related to the intestines;
- A sharp increase in frequency or, conversely, serious delays in urination. This is due to the growth of a tumor that puts pressure on the bladder. There may be blood in the urine;
- Constant severe weakness;
- Excessively fatigue;
- Excessive sweating for no apparent reason;
- A slight increase in temperature without signs of a cold (from 37°C to 37.8°C);
- Constant swelling of the limbs. This is especially true for the legs and feet;
The symptoms listed above are not a prerequisite, but their presence may indicate other serious diseases, including gynecological or sexually transmitted diseases. Therefore, you should not postpone your visit to the gynecologist.
Diagnostics
Diagnosis of cervical cancer consists of several stages:
- Examination by a gynecologist to detect oncology. It is necessary to undergo it 2 times a year;
- Scraping from the surface of the cervix for cytological examination (Papanicolaou smear);
- Colposcopy. An examination using a special device that helps to enlarge and zoom in on the tissue of the cervix;
- Biopsy - using this microinvasive method, biomaterial is taken for histological examination;
- The procedure for curettage of the cervical canal. It is necessary and carried out only in the case when cytology shows oncology or dysplasia, and colposcopy reveals nothing;
- Schiller test (with vinegar or iodine);
- Examination of the pelvic organs using ultrasound. Allows you to fairly accurately identify the presence or absence of tumor formations. If ultrasound is not enough to determine the exact location and quality of the tumor, then an MRI of the pelvic organs may be prescribed.
If there are several symptoms and serious suspicions of cervical cancer, the gynecologist may also prescribe related examinations regarding other organs to detect metastases:
- Ultrasound of the liver and kidneys;
- Ultrasound examination of the bladder;
- X-ray of the lungs. This is how distant metastases in the chest are detected;
- X-ray of the colon (irrigoscopy);
- Purpose of cystoscopy and rectoscopy. Examination data of the bladder and rectum make it possible to determine the presence of metastases or tumors that have penetrated their walls;
- Intravenous urography. Cervical cancer is often accompanied by compression of the ureters and leads to serious problems with the functioning of the kidneys. Up to the development of atrophy of the renal tissues or ureters. This method allows you to identify such violations.
Which doctors should I contact?
The main doctor who conducts examinations and prescribes treatment is a gynecologist. If cancer is discovered during the process, you will additionally need to be monitored by an oncologist. Doctors of other profiles (general practitioner, endocrinologist) are visited as needed or in cases of detection or development of other diseases.
Treatment
Treatment methods largely depend on the degree of development of the disease. Here you need to remember that, although there are only 5 stages of cancer (including zero), each of them has 2 - 3 degrees of complexity (category A or B). The designation depends on the size and location of the tumor:
- Stage 1A1. (invasive stage). The tumor is detected only by microscopic examination. The area affected is only the cervix (without metastases). The dimensions do not exceed 7 mm in volume and 3 mm in depth of the epithelium. Treatments include conization (excision of diseased tissue) in young patients or traditional hysterectomy (removal) of the uterus in postmenopausal women. If there is concomitant damage to the lymph nodes or blood vessels, lymphadenectomy (lymph nodes are removed) of the pelvic area is prescribed. After the operation, radiation therapy is prescribed (may be with or without chemotherapy);
- Stage 1A2 (invasive stage with complications). The tumor also cannot be detected visually, but when detected, it turns out that its dimensions exceed 7 mm in width and 3 mm in depth. Treatment for patients of childbearing age is cervical excision or conization, and for older patients, hysterectomy is prescribed. Pelvic lymphadenectomy is mandatory. If metastases are detected, chemotherapy and radiation therapy are performed;
- Stage 1B The tumor is visible visually, and its size does not exceed 4 cm. There can be 2 methods of treatment: surgery with external irradiation. In the first case, a radical hysterectomy (removal of the uterus completely with appendages and tubes) and bilateral oophorectomy are performed. A pelvic lymphadenectomy is required and performed. In especially favorable cases, surgical treatment is carried out with preservation of all organs. In the second case, the problem is solved by radiosurgery. First, brachytherapy is performed, and after 1.5 - 2 months - the operation itself;
- Stages 1B2 - 5A. the tumor is detected visually, and its size is equal to or slightly exceeds 4 cm. In such a situation, tumor damage to the vagina, rectum and bladder is possible. The most optimal treatment is radiation therapy and chemotherapy. ;
- Stage 5B. The affected area and overall size of the tumor can be any. Also at this stage there are distant metastases. At this stage, palliative treatment is carried out.
Observation after treatment
All patients who have been diagnosed with cervical cancer and received appropriate treatment must regularly visit a gynecologist and undergo the necessary instrumental and laboratory diagnostics.
For 2 years after treatment, a cytogram analysis must be performed every 3 months. For another 3 years after this, a smear is taken every six months. For the rest of your life, the cytogram is taken annually. This is necessary in order to avoid relapse of the disease.
To monitor the appearance or development of metastases, as well as for their early detection, MRI, CT and PET scans of the abdominal cavity and pelvic area are used.
Prevention
Vaccination against the papilloma virus (HPV), as the main source of cancer development, is recognized as the most effective prevention.
It can be done from 9 to 11 years of age, since the drugs are most effective if the vaccination is done before the start of sexual life. This means before infection with a sexually transmitted virus.
It also makes sense to vaccinate all women under 45 against this virus.
The most studied and effective means of immunization is the Gardasil vaccine. The drug effectively protects against the virus for 4 years after vaccination. Then the procedure must be repeated.
Source: https://www.polyclin.ru/rak-sheyki-matki/