It is unlikely that any modern gynecologist will agree to diagnose a woman without using modern research methods. The most accurate endoscopic method for diagnosing intrauterine pathologies is diagnostic hysteroscopy. This endoscopic examination helps many women find out about problems in their gynecological health.
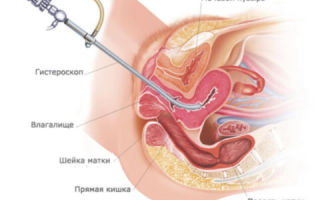
Hysteroscopy of the uterus refers to a procedure for examining the internal surface of the uterus. The procedure is carried out using a fiber optic device that projects the image on a monitor. The doctor moves the device clockwise to assess the condition of the fallopian tubes, endometrium and uterine cavity.
Diagnostic hysteroscopy is, although small, an operation. After all, to penetrate the uterus, it is necessary to expand the lumen of the cervix with mirrors. This requires local anesthesia.
Diagnostic hysteroscopy is called so because this method is the best for diagnosing most diseases of the uterine cavity. At the time of examination, a special probe with LEDs and a micro video camera is inserted into the uterine cavity (this is a hysteroscope).
During diagnostic (office) hysteroscopy, a specialist examines the lining of the uterus to confirm or exclude any disease suspected by the doctor.
This type of study is carried out on an outpatient basis. It is usually prescribed for the initial detection of diseases of the uterus or for monitoring gynecological diseases over time.
Office hysteroscopy usually does not exceed half an hour. Most often, this procedure is recorded on video . This can be convenient for comparative analysis of subsequent studies of the patient.
There is no need to use general anesthesia for diagnostic hysteroscopy. Such a study is absolutely safe, since it does not affect the internal uterine part.
Advantages of the method
More recently, for many problems with women’s health (bleeding, habitual miscarriage, chronic inflammation, etc.), diagnostic curettage (popularly “cleansing”) was prescribed. Compared to similar “blind” curettages and other invasive methods, endoscopic hysteroscopy has the following advantages:
- maximum diagnostic accuracy (up to 100%);
- low morbidity with extremely rare complications;
- painless and quick recovery after the study;
- carried out on an outpatient basis;
- the ability to take tissue for examination in a precisely planned location (targeted biopsy);
- optical control of all manipulations in the uterus;
- the possibility of treating uterine pathologies immediately after their diagnosis.
As you can see, this endoscopic method has many advantages over other methods that are less accurate in diagnosis (ultrasound) or more traumatic (diagnostic curettage).
Indications for hysteroscopy
In what cases does a doctor usually refer a woman for diagnostic hysteroscopy? Most often, a doctor prescribes this test if there is a suspicion of:
- infertility;
- frequent miscarriages;
- pathologies of the structure of the uterus or appendages;
- fistulas between the uterus and other organs;
- presence of fibroids;
- endometriosis;
- adenomyosis;
- suspicion of fragments of the fetal membrane remaining in the uterus (after childbirth);
- complications after childbirth;
- suspicion of a foreign object in the uterine cavity;
- any inflammation in the uterus;
- if you suspect the presence of any tumors (including submucosal fibroids);
- with bleeding of unknown cause;
- with irregular menstrual cycle (at any age).
For uterine fibroids, hysterography is generally irreplaceable. It is this diagnostic method that allows:
- determine the size of the nodes;
- clarify the location of nodal formations;
- choose a treatment method for this pathology.
Contraindications for the study
However, hysteroscopy may not always be used. This diagnostic method is contraindicated for:
- pregnancy (if there are no pathologies);
- heavy uterine bleeding;
- cervical canal cancer;
- narrowed cervix or cervical canal;
- any infections of the female genital area (in the acute stage or recently suffered);
- 3-4 degree of vaginal cleanliness;
- general infectious diseases with intoxication and high fever;
- impaired blood clotting;
- renal or heart failure;
- previous heart attack;
- oncological formations in the stage of decay or growth.
Preparing for the study
Although this research method is minimally traumatic, it still requires careful preparation. It happens that in the process of taking tests it turns out that hysteroscopy cannot be offered to a woman at the moment (for example, she has been diagnosed with a kidney or acute sexually transmitted infection, etc.)
Therefore, before this endoscopic method, a woman (no later than 2 weeks before hysteroscopy) must:
- Blood test (general, biochemical, coagulability, group determination, Rh factor).
- General urine analysis.
- Study of flora from the genital tract (smear for infection and oncocytology).
- Testing for dangerous infections (HIV, syphilis, hepatitis).
- Colposcopy.
- Ultrasound of the pelvic organs.
- Fluorography.
- ECG.
- Examination by a therapist.
- Based on the test responses received, the therapist makes a conclusion about the safety of hysterography for the patient and confirms consent to this type of study.
- During the conversation with the therapist, the patient must indicate that she is taking any medications.
- It is especially important to tell your doctor about the use of these medications:
- non-steroidal anti-inflammatory drugs;
- anticoagulants;
- blood thinners.
These drugs can cause bleeding and complicate hysteroscopy.
Before the study, it is necessary to prescribe certain medications to women who are at high risk of complications. In this case, antibiotics, antifungal drugs, and tranquilizers may be prescribed. The risk group includes women whose bodies are weakened due to diabetes, obesity, and chronic infections.
When is hysteroscopy performed?
Depending on the reason for the examination, endoscopy of the uterus may be prescribed:
- When gynecological diseases are detected - on days 6-9 from the start of menstruation (the first phase of the cycle). It is on these days that the condition of the uterine cavity is ideal for examination with a hysteroscope.
- If you suspect endometrial hyperplasia - any day.
- For intrauterine adhesions - before the onset of menstruation.
- To determine the cause of infertility (assessment of the functional uterine layer) - on the 20-24th day from the start of menstruation (the middle of the secretory phase). At this time, the condition and volume of the internal epithelium is clearly visible.
How to prepare for research
To undergo hysteroscopy, the patient must prepare as follows:
- Avoid using douches and do not use vaginal suppositories or tampons.
- Avoid sexual intercourse 2 days before the study.
- Take food no later than 19 pm, and water no later than 24 hours.
- Mandatory evening enema with clean water.
- Emptying the bladder before the study.
- Taking a shower, treating the pubis and perineum (shaving).
- Take antibiotics 2 hours before the test (to prevent complications).
- Taking mild sedatives for nervous excitement or anxiety (valerian, peony, motherwort).
- Take hygiene products with you (cotton socks and shirt, pads, towel, disposable sheet).
How does office hysteroscopy work?
Before the procedure, the doctor lubricates the patient’s genitals and thighs with an antiseptic solution. The cervix is fixed and treated with ethanol. Then a probe is inserted into the cervix, and its length is measured.
After dilation of the cervical canal, it is washed, and secretions are drained from it. Then the hysteroscope is inserted into the uterus, from where the mucous membrane and the shape of its cavity and relief are examined.
At the same time, data on the color, thickness and condition of the orifices of the fallopian tubes is analyzed.
The normal uterine cavity looks like an oval, with the thickness and vascular pattern of the endometrium according to the cycle:
- before ovulation, the endometrium is abundantly supplied with vessels;
- after ovulation, the endometrium becomes folded and thickened;
- before menstruation, the endometrium becomes thickened, velvety, with areas of hemorrhage.
What is revealed during hysteroscopy
Most often, endoscopy of the uterus reveals the following problems:
- Uterine fibroids : represented by myomatous nodes. It looks like tumors: light pink, round, with smooth edges, they can look like thickenings (protrusions) in the muscle layer. The issue of possible resection of nodes during subsequent hysteroresectoscopic myomectomy is often addressed.
- Formation of polyps : looks like an increase in the mucous membrane with outgrowths of the endometrium. Endometrial polyps can hang into the uterine cavity, be single or numerous. Often, during surgical hysteroscopy, polyps are also removed and sent for histology.
- Endometrial hyperplasia : based on the thickening of the uterine lining, which is measured. With diffuse hyperplasia, the possibility of malignant degeneration of individual growths is determined.
- Internal endometriosis (or adenomyosis) is often difficult to identify and requires sufficient specialist experience. They may appear as white spots with blood spots.
- Glandular endometrial cancer can be suspected and confirmed by histological examination of a piece of tissue. Often this is the only way to timely detect this type of neoplasm.
Hysteroscopy is the most revealing study: it is capable of 100% identifying polyps in the uterus.
Recovery period
Typically, examination with a hysteroscope has no consequences for the patient. Such patients do not need any medical supervision.
Complications and bleeding after hysteroscopy are extremely rare.
But still, after this procedure, the doctor usually gives the woman the following recommendations:
- temperature measurement;
- washing the genitals twice a day;
- exclusion of any stress and sex for a period of 2 weeks;
- taking antibacterial drugs to prevent the development of a bacterial infection;
- assessment of discharge after manipulation: short-term discharge of moderate volume is considered normal;
- to relieve possible pain, analgesics (Analgin, Ibuprom, Nimesil, Baralgetas) are used for 2-3 days;
- it is advisable to use birth control for 1-2 months after the procedure;
- It is not recommended to use vaginal tablets, suppositories or tampons for 2 weeks;
- For several days after the study, visiting a bathhouse, sauna, or swimming pool is undesirable, and bathing in a bathtub is better replaced with a shower.
All such precautions are necessary to prevent complications. Usually, by 3-5 days after the manipulation, the woman returns to her usual lifestyle.
Possible complications
Typically, office hysteroscopy rarely causes serious complications for women's health. Let's consider possible complications and help with them:
- Spastic pain in the lower abdomen. This is understandable, since the body underwent instrumental intervention. Here we can take analgesics.
- Flatulence after anesthesia. It is normal and goes away quickly.
- Bleeding. Scanty and spotting discharge after the procedure is considered normal. A violation is indicated if spotting lasts longer than two days after the manipulation. In this case, the doctor usually prescribes hemostatic and contracting drugs.
- Endometritis (inflammation of the uterine lining). Its symptoms are pain in the lower abdomen, bloody purulent discharge from the vagina. Treatment requires comprehensive treatment, using antibacterial drugs and eliminating intoxication.
The first menstrual bleeding after the procedure is not a pathology. If the discharge becomes purulent, abdominal pain and fever appear, you must consult a doctor!
Hysteroscopy before IVF
Hysteroscopy before IVF is very desirable, but not strictly necessary.
Office hysterography is especially often used for accurate diagnosis before in vitro fertilization surgery. Sometimes it is combined with a small curettage (therapeutic and diagnostic hysterography).
Diagnostic hysteroscopy before IVF allows you to choose the most optimal IVF protocol scheme and the most effective treatment method in cases of many disorders.
After all, even initially successful IVF does not always end in normal pregnancy and the birth of a full-fledged baby. And the reason for this is precisely the diseases of the female genital area that were not diagnosed in a timely manner and not cured.
Many intrauterine diseases of a woman can negate the expensive procedure of in vitro fertilization.
That is why it is best to conduct a hysteroscopic examination before repeated deaths occur during embryo transfer or termination of such a desired pregnancy. Until now, the ultrasound method has been used in this case. However, he is not able to identify all uterine pathologies in the initial stage.
The use of hysteroscopy during IVF allows:
- assess the patency of the cervical canal;
- cauterize erosion;
- diagnose undiagnosed endometrial pathologies;
- perform a cervical biopsy;
- remove polyps;
- cut the adhesions.
Hysterography is especially recommended before IVF for the following disorders:
- narrowing of the cervical canal (polyps, narrowing);
- intrauterine pathologies (hyperplasia, fibromatous nodes, endometriosis, dystrophy);
- several unsuccessful IVF attempts.
Beautiful women should not be afraid of office hysteroscopy or neglect this type of examination.
In many situations, this endoscopic method is simply irreplaceable, as it can promptly identify serious gynecological pathologies, which include glandular cancer of the uterus.
In other cases, the hysteroscopy method makes it possible to promptly identify and treat intrauterine pathologies, thereby facilitating the successful completion of an expensive IVF procedure.
Source: https://BornInVitro.ru/diagnostika-besplodiya/diagnosticheskaya-gisteroskopiya/
For what diseases is hysteroscopy indicated? Reviews from patients and doctors:
Hysteroscopy of the uterus is a fairly safe medical procedure performed using a special hysteroscope device. The endoscopy method was first used in 1869 to identify pathological changes in the uterine cavity. At that time, medicine was not so developed, so the device used to carry out the examination resembled a cystoscope. With the introduction of monitors and fiber optics, the possibilities have expanded significantly. Diagnostic hysteroscopy is used to examine and assess the condition of the uterine cavity. Feedback from women about this procedure is mostly positive. During the examination, the doctor can immediately identify the existing pathology and take action. Surgical endoscopy in gynecology is an intrauterine operation with disruption of endometrial tissue. A control test is prescribed after surgery in order to monitor the effectiveness of therapy. In any case, before the procedure, the patient must undergo the necessary tests to identify contraindications.
Examination technique
Hysteroscopy can be performed both under anesthesia (local/general) and without it. Reviews from some patients are negative. During medical manipulation (without pain relief), pain and unpleasant pulling sensations are felt in the abdominal area. The procedure itself does not take more than half an hour.
Diagnostic hysteroscopy is performed in 10-15 minutes. A thin tube with a diameter of no more than 5 mm containing an optical fiber is inserted through the vagina. After which the uterine cavity is filled with sterile liquid to facilitate access to the internal walls of the organ and to study its condition. If any pathologies are present, a biopsy (a piece of tissue) is taken.
The entire procedure can be recorded on video.
Indications
The method is actively used for infertility, as well as for frequent miscarriages. Medical manipulation is indicated for heavy bleeding that is associated with dysfunction of the appendages. The endoscopist recommends it for people with congenital or acquired uterine anomalies, as well as women with gynecological diseases. It is carried out if fibroids, endometriosis, polyps and malignant tumors are suspected. At an early stage, all diseases are especially well diagnosed, this increases the chances of a successful cure. Diagnostic hysteroscopy also helps to identify the true cause of an irregular and painful cycle.
Consequences and complications
Although this procedure is considered the safest, complications still occur in practice, and most often this is due to improper or careless implementation. Of course, the greatest number of negative consequences occur during surgical endoscopy as a result of long operations. Complications in the postoperative period are not excluded. The main negative consequences include: uterine bleeding (after removal of a fibromatous node or polyp), endometritis (inflammation of the mucous tissue as a result of pathogenic bacteria) and uterine perforation (damage or injury to the wall). In addition, hysteroscopy can exacerbate inflammatory processes (if they were not identified before diagnosis). Reviews from doctors report that this research method allows you to identify the disease at an early stage. To avoid negative effects, the procedure should only be performed by a qualified doctor after a complete examination of the patient.
Contraindications
Endoscopy is not performed for severe cervicitis, endometritis, cervical cancer, bacterial vaginosis and vaginitis. The procedure is prohibited during pregnancy and during uterine bleeding. It is very important to examine the vaginal smear for infectious diseases before starting the procedure.
According to experts, hysteroscopy is mostly performed without complications. Reviews from doctors confirm the safety and effectiveness of the examination. After the procedure, a woman may feel nagging pain in the abdominal area for several days. Scanty bleeding is also possible, which will disappear on its own after 2-3 days.
After endoscopy, you should not have sexual intercourse (check with your doctor for the timing).
Source: https://www.syl.ru/article/141455/mod_pri-kakih-zabolevaniyah-pokazana-gisteroskopiya-otzyivyi-patsientov-i-vrachey
Technique of hysteroscopy surgery
Hysteroscopy in gynecology is the most modern and high-tech method for assessing the condition of the female reproductive system. It allows you to conduct a thorough examination of the vagina, cervical canal, uterine cavity and fallopian tubes, diagnose diseases of the genital organs at the earliest stages and begin treatment long before the first symptoms appear.
What is a hysteroscope
A hysteroscope is an endoscopic optical medical instrument that is designed to examine the walls of the vagina, cervix and uterine cavity without incisions.
It consists of a tube that is equipped with an ultra-thin CCTV sensor with a light bulb. The sensor transmits an image enlarged several times to the monitor in real time.
Hysteroscopy is used to diagnose pathologies inside the uterus, as well as for a wide variety of gynecological operations.
A hysteroscope allows you to perform any surgical intervention under the visual supervision of a doctor. Thanks to this device, the risks of damage and complications associated with curettage and cleaning of the uterine cavity are minimized.
Indications
Indications when hysteroscopy of the cervix and uterine cavity for therapeutic purposes is necessary:
- endometrial growths - hyperplasia and other problems with the endometrium (endometriosis, adenomyosis);
- formations in the uterus and on the cervix - polyps, fibroids, cysts, etc.;
- the presence of adhesions in the uterus;
- oncological processes in the uterus and cervix;
- termination of pregnancy - abortion, curettage after pregnancy fading or miscarriage;
- diagnostic curettage of the uterine cavity;
- removal of the intrauterine device (in case of its ingrowth, when removing it by the wire threads is impossible);
- collection of material for histological examination;
- Diagnosis of difficulties with conception and pregnancy.
The advantage of hysteroscopy is the ability to combine a diagnostic procedure and gynecological surgery.
If the doctor has every reason to suspect the presence of a disease, it is possible to diagnose and, for example, remove the tumor in one session. To do this, the patient is immediately prepared for surgery, before which the surgeon performs the necessary diagnostic procedures.
Analyzes
After a hysteroscopy operation is prescribed, the woman will have to undergo a series of examinations:
- clinical and biochemical blood test;
- general urine analysis;
- smears for examination of vaginal microflora and cytological examination for atypia;
- coagulogram - test for blood clotting;
- blood test for HIV, syphilis, hepatitis B;
- electrocardiogram;
- fluorography (chest x-ray).
This is a standard set of tests for any gynecological surgical intervention.
Preparation
The doctor will prescribe a hysteroscopy operation 4-10 days after the start of menstruation. This is the best period for any surgical intervention or diagnostic examination in gynecology.
Hysteroscopy is contraindicated during pregnancy, since any manipulation of the uterus causes interruption or threat of miscarriage. If you suspect pregnancy, you must immediately inform your doctor.
Before surgery, the patient should:
- after consultation with your doctor, stop using suppositories and other medications;
- do not use soap and other alkaline intimate hygiene products for ten days;
- 2-3 days before the operation, refuse sexual intercourse;
- do not drink water or eat food in the evening, at least 10-12 hours before surgery.
How it goes
Hysteroscopy is performed in the morning. Before the procedure, primarily due to the use of anesthesia, you should not drink or eat. A patient scheduled for hysteroscopy is taken to the operating room.
There the woman is put into medicated sleep - most often general short-term intravenous anesthesia is used.
A thin hysteroscope tube is inserted into the uterus through the vaginal cavity and cervix, without incisions in the abdominal cavity or organs, and then the uterine cavity is filled with carbon dioxide or saline.
This allows you to straighten the walls of the uterus and improve visibility for examination and surgery. All instruments for the operation are inserted into the uterine cavity through a thin hysteroscope tube. This allows you to carry out all manipulations as carefully and accurately as possible. Throughout the entire period, the patient is under the supervision of an anesthesiologist.
The most gentle method is the use of a flexible hysteroscope during surgery. This device avoids the need for physical expansion of the cervical canal, which minimizes damage and complications.
However, a flexible hysteroscope cannot be used in situations where it is necessary to carry out a large volume of manipulations or remove large tumors.
The operation can take place both on an outpatient basis and in a hospital setting. Depending on how complex the surgical intervention was, the patient may be detained under the supervision of a doctor from two hours to several days.
Diagnostic minimally invasive hysteroscopy is often performed without the use of general anesthesia, with or without local anesthesia. In this case, the woman will be able to go home immediately after the operation.
The operation on average lasts no more than 40-60 minutes. The time depends on the doctor’s experience, as well as the scope of surgical procedures in a particular case.
Postoperative period
After surgery, women most often experience slight bloody (red and brown) vaginal discharge that goes away within a few days.
You may experience pain and cramping in the lower abdomen, which will go away on its own in a few days.
If you experience severe cramps and no effect of painkillers, you should consult a doctor.
Severe breakthrough bleeding after hysteroscopy is very rare. Such a symptom, depending on the patient’s condition, requires immediate examination by the treating gynecologist or calling an ambulance.
Contraindications
Hysteroscopy, like any surgical intervention, is not performed in case of problems with blood clotting, with inflammatory processes in the active stage in the pelvic area (bacterial vaginosis, sexually transmitted diseases, urethritis, cystitis and others), with renal or heart failure, during an acute respiratory viral infection.
Surgery during pregnancy is possible only if it is necessary to terminate it. In cases with a normally developing pregnancy, it is a contraindication for hysteroscopy.
Hysteroscopy of the uterus is a modern and simple way to treat a large number of female diseases.
Thanks to a high-resolution camera and color images on a monitor in real time, doctors no longer perform gynecological operations blindly.
The video image allows you to control the surgical process with high precision and even save it in photo and video format for further monitoring of changes and the course of the postoperative period.
Source: https://ginekola.ru/ginekologiya/matka/v-kakih-sluchayah-naznachayut-operaciyu-gisteroskopiya.html
On what day of the cycle is it better to do hysteroscopy and how is the procedure performed?
Uterine hysteroscopy is a non-invasive method for diagnosing and treating gynecological diseases. When a woman is prescribed this procedure, she has a number of questions, and the most popular remains interest in the date of its implementation. In medicine, there are certain standards for which day of the cycle hysteroscopy is performed.
The choice of the phase of the menstrual cycle when it is better to do an examination, curettage or removal of tumors is carried out taking into account the diagnosis. Therefore, a woman will not be able to undergo hysteroscopy at any time. The doctor will have to determine the most suitable day of the menstrual cycle for the procedure, and you will have to agree with his conclusions, even if the date turns out to be “inconvenient”.
Types of hysteroscopy
The first thing that affects the timing of hysteroscopy is the type of intervention, which can be diagnostic and operational (therapeutic). Diagnostic hysteroscopy is divided into several types:
- survey, during which only a camera is used to examine the uterus;
- with the collection of material, which is performed by scraping or pinching off a small fragment of tissue.
Visual diagnostics are done at a time when it is possible to examine the organ from the inside as accurately as possible, and at the same time its walls will be less susceptible to injury. This is usually the phase immediately after the end of menstruation. If it is necessary to obtain the endometrium for a comprehensive examination of the uterus, the procedure is postponed until the last days of the cycle.
A surgical procedure or hysteroresectoscopy is used to eliminate organ pathologies: septa in the uterus (synechia), polyps, small fibroids. On which day of the cycle it is best to perform hysteroresectoscopy is determined individually depending on the diagnosis and current condition of the patient.
- Before prescribing hysteroscopy, the gynecologist examines the patient in a gynecological chair and questions her about the timing of menstruation.
- Based on the preliminary diagnosis, a decision is made on which day of the cycle a hysteroscopy is performed.
- In order for the diagnostic procedure to be reliable, and for the therapeutic intervention not to result in complications, special preparation for hysteroscopy is required. It includes:
- laboratory diagnostics - the patient needs to undergo general urine and blood tests, as well as tests for sexually transmitted infections (smear) and blood tests for HIV;
- general instrumental studies - ultrasound of the uterus, fluorography, ECG;
- therapist's conclusion.
After determining the final date for hysteroscopy, the gynecologist advises the patient on the rules for preparing the genital tract for the procedure.
If the preliminary diagnosis revealed inflammatory or infectious processes, she will have to undergo treatment and then plan an intervention.
If the tests and results of instrumental studies are normal, the doctor will tell you what you can do on the eve of hysteroscopy and what you should avoid. So, the list of undesirable actions includes:
- intimate relationships 2-3 days before the scheduled procedure;
- taking a bath and douching a week before hysteroscopy;
- use of vaginal suppositories with antibiotics a week before manipulation.
On the eve of hysteroscopy, it is necessary to begin cleansing the intestines. In the morning it is forbidden to drink and eat.
Hysteroscopy is indicated in the presence of many pathological changes in the uterus:
- to identify and treat diseases in the field of gynecology that have caused infertility, spontaneous abortion or intermenstrual bleeding;
- in the presence of fibroids and endometrial polyps (the procedure is carried out to detect neoplasms, and if necessary, a polyp in the uterus is removed in one procedure);
- with endometrial hyperplasia;
- with congenital pathology of the uterus (bicornuate uterus, septum in it, etc.);
- with internal endometriosis, when endometrioid cells have affected the mucous membrane of the cervical canal.
- Hysteroscopy also has extensive contraindications, which are in one way or another related to the state of the endometrium and the general health of the genitourinary system.
- By standards, any inflammatory and infectious disease is a relative contraindication.
- If hysteroscopy is necessary, preliminary therapy is carried out, and then intervention is prescribed. Gynecologists consider the following to be absolute contraindications:
- severe heart defects and organ failure that prevent the use of anesthesia;
- HIV;
- pregnancy;
- a cancerous tumor that has affected the lining of the cervical canal.
Hysteroscopy is not performed during bleeding, including menstrual bleeding, or during cervical stenosis.
Scheduled hysteroscopy on which day of the cycle is performed depends on the purpose of its implementation and the preliminary diagnosis.
If it is prescribed for the diagnosis and removal of tumors in the uterine cavity, it is advisable to carry out manipulations on the 4th day of the cycle, that is, immediately after the end of bleeding.
Patients whose periods last more than 3 days can undergo hysteroscopy on the 5th, 6th and even 9th day of the cycle.
The procedure, designed to determine the functionality of the endometrium, is carried out in the second phase of menstruation or at the end of the cycle. This is due to the fact that on the 15th day of the cycle the endometrium thickens and all its flaws become visible. You can conduct an examination both on the 16th and 18th day, but not a day later, since the endometrium becomes too loose.
In case of emergency situations, it does not matter which day of the cycle the study will be carried out. For example, diagnosing and eliminating perforation of the uterus does not involve long calculations and waiting for a deadline according to the schedule, until what day of the cycle can perforation of the organ wall be detected and eliminated.
Important! If there is a suspicion of organ rupture, placenta accreta, or the presence of fetal egg remnants in the uterus, intervention is carried out urgently after the bleeding has stopped.
Even if the gynecologist decided to do a hysteroscopy on the most favorable day of the cycle, the risk that the procedure will affect future menstruation remains. Regardless of the phase in which the manipulations were performed, the body needs time to restore the uterine tissue. Therefore, the days of the cycle in subsequent months may be slightly shifted.
Shifts in the DC are especially noticeable when large tumors and uterine fibroids are removed.
There is no need to worry about this, since complete recovery sometimes takes up to three cycles. If menstrual bleeding continues irregularly for more than 3-4 months, it is necessary to undergo additional examination.
Recovery after a hysteroscopy procedure takes from a week to 1-3 months, depending on the type of procedure and compliance with the doctor’s recommendations during rehabilitation.
In the first days, the patient's condition may be complicated due to abdominal pain, which can be easily relieved with antispasmodics. Taking drugs in this group is very important for the prevention of cervical stenosis.
To prevent infectious complications, the gynecologist prescribes antibiotics.
Another problem that patients may encounter is prolonged bleeding or spotting. Typically, this situation occurs if curettage was performed in the second phase of the menstrual cycle.
Prolonged bleeding is not considered a pathology if its duration does not exceed 10 days.
Source: https://radiomarkett.ru/kakoy-den-vypisyvayut-posle-gisteroskopii/
Hysteroscopy: causes, symptoms, diagnosis and treatment in Moscow
Hysteroscopy is a method of treating and diagnosing diseases in the uterine cavity. It is used in gynecology as a low-traumatic method of examining and treating diseases of the uterus.
Types of hysteroscopy
There are diagnostic, control and surgical hysteroscopy.
Diagnostic hysteroscopy is performed with a hysteroscope - a special device equipped with an optical fiber. One part of the hysteroscope is inserted into the uterine cavity through the vagina and cervical canal, the other remains in the hands of the doctor.
The device displays an image from the cavity on a screen, and the gynecologist can carefully examine the cervical canal and the uterine cavity from the inside, including the openings of the fallopian tubes, and identify the presence of pathological changes, such as polyps.
There are various optical systems built into the hysteroscope. Some of them allow you to enlarge the image of the endometrium from the uterine cavity by 20 times.
This way the doctor can detect the slightest changes in the endometrial tissue and mucous membrane of the cervical canal. Some systems allow you to magnify the image a hundred times and even examine epithelial cells.
This is important when diagnosing neoplasms in the uterine cavity if there is a suspicion of cancerous degeneration of endometrial cells.
A surgical hysteroscope has built-in surgical equipment in addition to optical equipment. Under optical control, the gynecologist removes defects on the walls of the uterus and at the entrances to its appendages. Visual inspection of the cavity allows you to minimize surgical intervention and remove defects as carefully as possible. As a result, endometrial tissue heals faster.
Hysteroscopy has undeniable advantages over analog methods of diagnosis and treatment:
- does not require significant expansion of the cervical canal (the canal connecting the vagina to the uterine cavity), so there is no risk of cervical rupture during examination or treatment;
- the likelihood of damage to the mucous membrane of the uterine walls is extremely low, since all surgical procedures are carried out under visual control;
- There is virtually no pain during diagnosis; women may feel some discomfort during dilation of the cervical canal, but not pain.
When is hysteroscopy performed?
Hysteroscopy is one of the most commonly used instrumental methods of gynecological diagnosis.
Diagnostic hysteroscopy is recommended to be performed in the first half of the cycle, when menstrual bleeding has already ended. The best time is the fifth or sixth day of the female cycle.
At this time, the thickness of the endometrial layer is minimal, and the doctor has the opportunity to examine the uterine cavity as best as possible.
If an urgent examination of the uterine cavity is required, it is carried out on any day, regardless of the menstrual cycle.
Diagnostic hysteroscopy is performed when there is a suspicion of the following diseases:
Symptoms of these diseases may include heavy menstrual or intermenstrual bleeding, spotting of unknown origin, pain in the lower abdomen and lower back, inability to conceive or bear a child, pain or discomfort during sexual intercourse.
Hysteroscopy is also recommended after surgical or medical abortion or spontaneous abortion to detect the remains of fetal membranes in the uterine cavity. It is also indicated when a woman suffers from heavy and painful menstruation in the absence of other visible symptoms.
Control hysteroscopy is used to assess the condition of the uterine cavity after treatment. For example, after serious hormonal treatment, hysteroscopy helps to evaluate changes in the endometrium.
Doctors resort to surgical hysteroscopy to treat various pathologies of the uterine cavity, for example, intrauterine polyps. It helps to remove tumors and the overgrown layer of the endometrium while minimally injuring the organ.
What diseases are treated with hysteroscopy?
Hysteroscopy can be used as an independent treatment method or combined with other methods. It is usually combined with curettage (curettage).
Therapeutic hysteroscopy is performed:
- for polyps on the walls of the uterus;
- with thickening (hyperplasia) of the endometrium;
- with endometriosis;
- with fibroids;
- with regressive (frozen) pregnancy;
- ectopic pregnancy or when the fetus is located at the exit of the fallopian tubes;
- the formation of adhesions in the uterine cavity, for example, during the fusion of the walls of the uterus or the formation of partitions inside the organ;
- ingrowth of intrauterine contraceptives (coils, loops, rings) into the tissue of the uterine walls.
Hysteroscopy can also be used to terminate early pregnancy. For abortion in late pregnancy, hysteroscopy can be used as an auxiliary method.
Preparation for hysteroscopy
Preparation for hysteroscopy begins during examination by a gynecologist. The patient is examined using a speculum, and a vaginal smear is taken for bacteriological culture. In some cases, a cervical smear may be required. This is necessary to detect infection.
Before hysteroscopy, the patient undergoes a series of laboratory tests. The doctor prescribes tests after listening to the woman’s complaints and preliminary outlining possible diagnoses.
The doctor may prescribe an ultrasound of the uterus and appendages. Ultrasound will help assess the thickness of the mucous membrane, identify overgrown epithelium or inflammation, and find neoplasms or the fetus during pregnancy. Hysteroscopy will help clarify the diagnosis made after ultrasound.
Immediately before the procedure, it is recommended to empty the intestines and bladder.
If surgical hysteroscopy is prescribed under general anesthesia, you should not eat 6 hours before the procedure and drink 4 hours before the procedure. These are general requirements for operations performed under general anesthesia.
Before surgery, the patient should talk with the anesthesiologist and talk about any allergies to medications. The anesthesiologist will select the drug and calculate the dose. You also need a consultation with a cardiologist and a therapist: they will assess the woman’s general condition and the risks of anesthesia and the procedure.
Progress of the procedure
Hysteroscopy is considered a minimally invasive method of examination and treatment, and therefore takes place without hospitalization. Diagnostic procedures are performed without anesthesia. Patients who have undergone examination with a hysteroscope note that the procedure is painless. Sometimes, at the request of the patient, local anesthesia can be used.
Surgical hysteroscopy requires general anesthesia. The anesthetic is administered immediately before surgery, when the woman is already on the operating chair or couch.
After pain relief, the doctor opens the cervix. The degree of expansion required is small, since the device is quite miniature. After dilating the cervical canal, a part of the hysteroscope is carefully inserted into the cavity.
This is a soft hollow tube or a thin hard wire with a slight expansion at the end. This extension contains the optical fiber and the light source. The other part of the hysteroscope remains in the hands of the doctor.
The hysteroscope is connected to a large monitor, on which the image is displayed.
A solution or gas mixture is introduced into the uterine cavity through a hollow tube, expanding the uterine cavity and the mouth of the fallopian tubes. After expansion, you can better see each part of the inner lining of the organ and its exits. The doctor gradually moves the hysteroscope inside the uterus, examining each part of it. It is possible to magnify the image a hundred times, which allows you to examine the endometrial cells.
If hysteroscopy is performed for diagnostic purposes, this is where the procedure ends.
If treatment is required, surgical equipment is inserted through the hysteroscope, pathological formations or an overgrown endometrial layer (hyperplasia) are removed.
After completion of the procedure, the solution is removed from the uterine cavity. If necessary, the doctor injects a drug into the uterus. Next, the hysteroscope is carefully removed from the uterus through the vagina.
Rehabilitation
After diagnostic hysteroscopy, a woman may feel nagging pain of moderate intensity in the lower abdomen. This is how the muscular layer of the uterus reacts to external invasion of a foreign object. The sensations are reminiscent of menstrual pain. If the sensations are very unpleasant, you can take an antispasmodic drug.
A slight discharge of blood after manipulation with a hysteroscope is also considered normal, especially after surgical removal of pathological areas. Bloody discharge should stop within 2-4 days. Women with poor blood clotting may need hemostatic medications.
After surgical hysteroscopy, the doctor prescribes antibiotics (to prevent postoperative inflammation). Other medications may be prescribed depending on the diagnosis.
For successful recovery after the procedure, a woman must follow a gentle regimen. Physical activity such as going to the gym or running is prohibited for 2 weeks. You cannot swim in the pool or take a bath - this can cause tissue infection through water. You should also avoid the sauna. It is better to replace tampons with sanitary pads during menstruation.
After hysteroscopy, a complete, vitamin-rich diet is indicated. Food should be light and slightly laxative to prevent constipation.
A few days after the operation, the gynecologist conducts a follow-up examination. He finds out how the tissue is healing and whether the pathological formations have been completely removed. The examination also shows whether there are any complications after the procedure.
Complications
Hysteroscopy is a minimally invasive method in gynecological surgery, so the likelihood of complications is quite low. The most likely complications of hysteroscopy are:
- increased bleeding;
- endometritis (inflammation of the endometrium);
- menstrual irregularities;
- cervical rupture;
- perforation of the uterine wall;
- incomplete removal of pathology, for example, polyps.
A slight disruption of the cycle after surgical hysteroscopy is allowed. This is how the body reacts to the operation; it needs time to recover before ovulation. A prolonged absence of menstruation after hysteroscopy should alert the patient; the doctor should be informed about this and the cause should be found.
Contraindications
Even the safest procedure has contraindications, and hysteroscopy also has them. This method should not be used during pregnancy, as it can cause miscarriage or damage the membranes.
For inflammatory and infectious diseases, hysteroscopy is not performed so as not to transfer the infection from the vagina to the uterine cavity and above. The closure of the cervix and the mucous layer at the base of the cervix prevent the penetration of bacteria and fungi from the vagina. A hysteroscope can open a passage for infection and make the infection worse.
In case of heavy uterine bleeding, hysteroscopy is not performed, as it may increase the bleeding, and the abundance of blood in the cavity will not allow the doctor to examine the organ properly.
Source: https://www.polyclin.ru/gisteroskopiya/
Hysteroscopy of the uterus will reveal intrauterine pathologies
Hysteroscopy is a visual examination of the uterus and cervical canal using specialized optical equipment. The procedure significantly expands diagnostic capabilities when assessing the condition of the uterus and treating pathological processes.
The procedure not only allows you to accurately diagnose intrauterine pathology, but also makes it possible to perform simple operations without incisions and trauma to surrounding tissues.
What is hysteroscopy and its types?
Today, this effective method of endoscopic diagnosis is used to identify intrauterine pathologies in most gynecological hospitals.
There are several types of hysteroscopy, depending on the goals and objectives of the doctor:
- diagnostic involves examining the inner surface of the uterus using optical instruments. The procedure allows you to determine the presence or absence of a pathological process. The integrity of the tissues during the diagnostic study is not compromised;
- surgery is performed for the purpose of atraumatic endoscopic intervention and surgical treatment of various intrauterine pathologies. In particular, surgical hysteroscopy is used to successfully remove polyps and myomatous nodes;
- control is necessary to monitor the progress of treatment. The examination allows us to identify its effectiveness, timely record relapses, and monitor the condition of the uterus after surgical or conservative therapy.
Microhysteroscopy allows for high-precision endoscopic operations due to multiple image magnification.
To conduct such an examination, a prerequisite is dilation of the uterine cavity through liquid or gas media. Depending on the stretching method used, liquid and gas hysteroscopy are distinguished.
To do this, doctors use carbon dioxide, saline, dextran, dextrose solution, sorbitol, and sterile water.
All media used provide the best visualization during the examination, being absolutely safe for the patient.
Why is hysteroscopy prescribed?
Among the indications for hysteroscopy are the following pathologies that require confirmation of diagnosis, monitoring and treatment:
- endometrial polyps;
- endometriosis;
- myomatous nodes;
- intrauterine synechiae;
- endometrial hyperplasia;
- various physiological defects of the uterus;
- suspicion of the presence of a foreign body or perforation of the uterine walls;
- suspicion of a malignant tumor;
- intrauterine fistula;
- dysmenorrhea;
- adhesions in the uterine cavity.
An examination is often prescribed for infertility. Hysteroscopy before IVF (in vitro fertilization) allows you to assess the condition of the uterus and ensure its physiological readiness for the procedure.
Relative indications for hysteroscopic examination may include bloody discharge from the genitals, irregular menstruation, primary miscarriage, as well as monitoring after hormonal therapy.
Contraindications to hysteroscopy
There are a number of pathologies for which endoscopic diagnosis is unacceptable:
Preparation for surgery and necessary tests
Before the procedure, the patient must undergo a mandatory gynecological examination.
The initial examination helps the doctor assess the condition of the vagina and vestibule of the cervix, as well as exclude the presence of infectious lesions of the genital organs.
During the examination, the doctor takes tests for hysteroscopy (a bacteriological smear from the vagina, as well as a smear for oncocytology). Test results are required to exclude the presence of absolute contraindications to the procedure.
Rules for preparing for hysteroscopy of the uterus:
- do not use vaginal suppositories, suppositories, sprays and other medications, as well as intimate hygiene products for a week before the procedure;
- abstain from sexual intercourse for two days before the test.
On what day is hysteroscopy performed?
Depending on the indications, the study is carried out in different phases of the cycle. If the procedure is prescribed to diagnose uterine adenoma or fibroids, the study must be carried out in the first phase of the menstrual cycle (several days after the end of menstrual bleeding). In the second phase of the cycle, hysteroscopy is performed to diagnose infertility and endometriosis.
For control and diagnostic hysteroscopy, hospitalization is not required, but in the case of surgery, the procedure is most often performed in a hospital setting.
How is hysteroscopy performed?
Using special devices, the doctor assesses the length of the uterus and expands the cervical canal, after which he inserts a hysteroscope connected to the fluid supply system into the uterine cavity.
Moving the hysteroscope clockwise, the doctor examines the mouths of the fallopian tubes, assesses the condition of the endometrium, the shape and relief of the uterine cavity.
Video: “What is uterine hysteroscopy? Preparation, implementation and rehabilitation. Hysteroscopy and IVF"
Recovery after hysteroscopy and general recommendations
In most cases, the procedure is easily tolerated by patients. Diagnostic hysteroscopy does not require additional observation and further rehabilitation, and is also very rarely accompanied by pain and bleeding.
If surgical hysteroscopy was performed, the patient requires medical supervision for some time after completion of the procedure. To prevent the development of bacterial infections, antibiotics of various pharmacological groups are prescribed.
Additionally, the nature of bloody discharge after hysteroscopy of the uterus is assessed. Most often, bleeding is moderate in nature, and after a while it disappears completely. Scanty vaginal discharge after the procedure is not a cause for concern.
To relieve pain, doctors recommend taking over-the-counter painkillers (Ibuprofen, Analgin, Baralgin) in the first days after surgery.
Painkillers should only be taken if there is severe pain. For mild pain in the lower abdomen, additional treatment is not required.
Minor pain after hysteroscopy goes away on its own within a couple of days.
If a woman is prescribed a curettage procedure, doctors recommend preventing pregnancy for several months. The most optimal period for pregnancy after hysteroscopy with curettage is at least a year after the procedure.
Recommendations after hysteroscopy:
- sex after hysteroscopy is unacceptable for a couple of days after the examination;
- stop using tampons, suppositories and vaginal suppositories;
- You should refrain from visiting baths, saunas, and swimming pools. Taking a bath is not recommended;
- 3 days after the procedure, the patient can return to her usual regimen.
Possible complications and consequences of hysteroscopy
Hysteroscopy is a safe diagnostic procedure, after which there are practically no complications. In rare cases, after the study, an infectious lesion of the uterine cavity is observed. In rare cases, severe uterine bleeding is observed.
Heavy periods after hysteroscopy are not a pathological consequence of the procedure, however, if heavy purulent and bloody discharge appears in the middle of the cycle, accompanied by fever and severe pain, you should consult a doctor.
Hysteroscopic picture and possible pathologies
Picture of a hysteroscopic examination of a healthy woman:
- in the first phase of the cycle, the endometrium has a uniform pale pink color and small thickness. At later phases of the cycle, the vascular pattern of the endometrium becomes less noticeable, and folds form on the surface of the endometrium. The color intensity of the endometrium intensifies in the last phase of the cycle;
- The uterus normally has a smooth oval shape. The orifices of the fallopian tubes are clearly visible at the beginning of the cycle, until the endometrium is thickened. With various intrauterine pathologies, the hysteroscopic picture changes.
With endometrial atrophy, the uterine mucosa has an uneven color, and areas of hemorrhage may be observed on it. The endometrium is thin, blood vessels are visible through it.
With submucous fibroids, examination reveals a rounded neoplasm protruding into the uterine cavity. The myomatous node has clearly defined contours and a uniform pale pink tint.
- Hyperplasia is characterized by uneven thickening of the endometrium, which acquires an uncharacteristic bright pink color.
- Endometrial cancer is characterized by the development of large folds and polyp-like formations, prone to contact bleeding.
- Endometrial polyps are represented by multiple neoplasms with a pronounced vascular pattern, protruding into the uterine cavity and having an irregular shape.
During examination, intrauterine synechiae are determined in the form of fragments of fibrous tissue that do not have a vascular pattern. Synechiae reduce the volume of the uterus and limit visual access to its corners.
If the patient is suspected of having a malignant tumor, additional histological examination of the tissues is necessary to clarify the diagnosis.
Hysteroscopy of the uterus: estimated prices
How much does hysteroscopy cost? The cost of the procedure depends on the type of clinic and the region in which the operation is performed. The cost of the procedure is also affected by its complexity.
Prices for diagnostic and control hysteroscopy vary on average from 4-9 thousand rubles. Surgical hysteroscopy will cost the patient more: prices for endoscopic surgery reach 13-20 thousand rubles.
Hysteroscopic examination is a safe, low-traumatic and virtually side-effect-free procedure that significantly expands the arsenal of diagnostic techniques in modern gynecology.
The procedure does not disrupt the woman’s reproductive function and does not affect the woman’s ability to further conceive children. Today, hysteroscopy is one of the most important techniques protecting women's health.
Source: https://ladyinform.com/gisteroskopiya-matki