All materials on the site were prepared by specialists in the field of surgery, anatomy and specialized disciplines.
All recommendations are indicative in nature and are not applicable without consulting a doctor.
Averina Olesya Valerievna, candidate of medical sciences, pathologist, teacher of the department of pathological anatomy and pathological physiology
Prostatectomy is considered a high-tech urological operation, which consists of complete removal of the prostate gland along with the capsule, seminal vesicles, pelvic tissue and lymph nodes.
The need for radical prostatectomy arises in case of serious pathology of the gland - cancer, severe hyperplasia, abscessing prostatitis. The operation is complex and requires the participation of an experienced surgeon, whose technique and skills largely determine the outcome and quality of life of the patient.
The prostate is a small gland of the male reproductive system, located at the bottom of the bladder and secretes a secretion that is part of sperm. It covers the outside of the initial portion of the urethra, so the pathology of the organ is accompanied by dysuric disorders.
The type of surgical technique for prostatectomy depends on the disease and condition of the patient; whenever possible, preference is given to laparoscopy, but such a serious condition as cancer often leaves no choice and forces the surgeon to resort to abdominal surgery.
Indications and contraindications for prostatectomy
Like any other operation, prostatectomy has certain indications and contraindications. The following are considered indications:
- Prostate cancer (the most common reason for organ removal);
- Acute prostatitis with the formation of phlegmon or abscesses in the pelvis;
- Chronic prostatitis with suspected carcinoma;
- Prostatitis with the formation of stones in the gland;
- Severe stages of prostate hyperplasia.
Prostatectomy is a traumatic intervention that requires general anesthesia, so it has contraindications, including the general serious condition of the patient, decompensated pathology of internal organs, age over 70 years, and bleeding disorders. An obstacle to prostate removal can be the inflammatory process in the pelvis in the acute phase, when the risk of infection and postoperative infectious complications is high.
If a patient is taking blood-thinning drugs, surgical treatment can be performed only 1-2 weeks after their discontinuation. If it is necessary to perform a planned prostatectomy, all diseases, if possible, are brought to such a course that the operation will not cause serious complications.
Types of prostatectomy
- The purpose of the operation to remove the prostate is to completely remove the organ with the seminal vesicles, part of the urethra, bladder neck, surrounding tissue and, if cancer is suspected, the pelvic lymphatic system.
- The differences in the techniques lie only in the access through which the surgeon reaches the affected organ.
- Highlight:
- Retropubic prostatectomy;
- Perineal;
- Laparoscopic.
retropubic prostatectomy
Retropubic prostatectomy is performed through the anterior abdominal wall. The surgeon makes an incision from the navel to the pubic junction, enters the abdominal cavity, reaches the prostate, crosses and ligates the vessels and nerves and removes the gland as a single block with the capsule, fiber, and seminal vesicles.
At the end of the operation, the doctor connects the neck of the bladder and the urethra, then sutures the tissue layer by layer. A catheter is installed in the bladder to drain urine, which remains there for up to 10-14 days. During this period, healing will occur at the site of the removed gland, and urine will be discharged through the catheter.
Drains are placed in the pelvis to drain wound fluid.
The operation lasts up to 3-4 hours. It is important to preserve the nerve fibers that provide urinary control and erection. This approach allows this to be done in most patients. If it is impossible to preserve these nerve bundles, various types of plastic surgery are used with the supply of nerve roots from neighboring areas.
perineal prostate removal
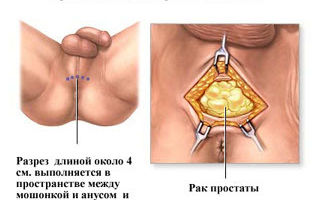
Perineal removal of the prostate is carried out by cutting the tissue of the perineum, between the scrotum and the anus.
Through this access, the surgeon removes the prostate gland with seminal vesicles, but this intervention option does not allow preserving the nerves responsible for erection and urinary retention.
The positive side of this method of prostatectomy is considered to be a good cosmetic effect, because the suture in the perineum is not visible to others.
If perineal prostatectomy is performed due to cancer, then there is a need for an additional incision in the abdominal wall to remove the pelvic lymph nodes. The perineal approach is used less and less, giving way to other methods that allow preserving the innervation of the pelvic organs with the least cosmetic defect.
Laparoscopic prostatectomy is successfully used in urological practice. The operation is low-traumatic, but allows you to remove the entire required amount of tissue.
During laparoscopy, the surgeon makes several incisions on the anterior abdominal wall, through which instruments, a video camera, and a light source are inserted.
Controlling the manipulations using a video camera, the surgeon removes the prostate gland, seminal vesicles, and lymph nodes.
All prostatectomy methods require general anesthesia and take from 2 to 4 hours. The operation is completed by suturing the soft tissues and leaving drains in the pelvic cavity. Immediately before surgery, antibiotic therapy is prescribed to prevent infectious complications.
Preparing for surgery to remove the prostate
When surgery is unavoidable, it is important to properly prepare the patient for the procedure to reduce the likelihood of complications and surgical risks.
The majority of patients in need of radical prostatectomy are elderly men suffering from a variety of somatic pathologies - hypertension, diabetes, atherosclerosis, chronic diseases of the bronchopulmonary system, etc.
, therefore, a thorough preoperative examination should be carried out and the treatment of these conditions should be adjusted if necessary.
The examinations required for prostatectomy are carried out on an outpatient basis, usually at the patient’s place of residence. The doctor determines a list of necessary procedures, which may take one to two weeks to complete.
Before the operation:
- General and biochemical blood tests, urine tests;
- Coagulogram;
- Tests for syphilis, HIV infection, hepatitis B and C;
- ECG (always for mature and elderly patients);
- Fluorography or chest x-ray.
If cancer is suspected, a study of the level of prostate-specific antigen is required; if metastasis is possible, bone scintigraphy is required. Usually, by the time preparation begins, the patient has already undergone a prostate biopsy; if not, that is also performed.
To clarify the nature of the pathological process, a digital examination of the prostate, an ultrasound examination of the pelvic organs (with a transanal sensor), CT and/or MRI of the affected area are performed.
When the necessary procedures have been completed, the patient is sent to a therapist, who gives his permission for the operation, taking into account the concomitant pathology. The anesthesiologist, based on the analysis data, determines the type of anesthesia and possible risks.
Having all the examination results and permission for surgical treatment from the therapist, the patient is hospitalized.
Before the operation, some studies may be performed again: ultrasound, coagulogram (especially in the case of previous use of anticoagulants).
The surgeon talks to the patient, explains the essence of the upcoming operation, the possible consequences, and the already informed patient signs his consent to the treatment.
On the eve of the operation, the perineum and abdominal wall are carefully and thoroughly shaved; after six o'clock in the evening, food and liquid intake is prohibited. Before prostatectomy in the evening, it is advisable to do a cleansing enema. On the morning of the intervention, antibiotic therapy is prescribed.
Postoperative period
At the end of the operation, the patient is taken to the recovery room or intensive care unit, where recovery from anesthesia, the condition of the wound, and drainage output are carefully monitored. If circumstances are favorable, the patient is transferred to the urology department on the second day, where the recovery period begins.
Before removing the sutures, the postoperative wound is treated with antiseptics twice a day, the urethral catheter is washed with a furatsilin solution to disinfect and prevent its blockage.
Sutures are removed on days 5-7, drainages are removed on days 4-5 after surgery. The urinary catheter is left in the bladder for up to 2-3 weeks.
This is necessary to restore urethral patency and heal sutures.
Recovery after laparoscopic surgery takes minimal time - up to several days, and with abdominal radical prostatectomy it can reach 2-3 weeks, during which the patient will have to stay in the hospital.
Drug treatment involves the prescription of painkillers, antibiotics, and anti-inflammatory drugs.
The next day after the intervention, food and liquid intake is already possible, early activation of the patient is encouraged - you need to get up and walk around the ward and corridor.
Movement contributes to a faster recovery and the prevention of many complications, including such dangerous ones as thrombosis and thromboembolism.
Prostatectomy may be accompanied by complications, the most likely of which are:
- Bleeding in the pelvis, the prevention of which is careful hemostasis and a Foley catheter installed in the bladder;
- Infectious and inflammatory processes accompanied by fever, pain, and general intoxication. Their prevention is antibiotic therapy, treatment of sutures and catheters with antiseptics;
- Urethral strictures with urination problems, for the prevention of which a good drinking regime is recommended;
- Thromboembolic complications, the risk of which is present in any operation, and to avoid them requires early activation, careful monitoring of blood clotting and even drug correction.
Frequent consequences of prostatectomy include urinary incontinence, impotence and erectile dysfunction. Urinary incontinence can persist for quite a long time and in some cases requires additional plastic surgery.
Serious psychological discomfort in men who have undergone prostatectomy causes impaired potency. Damage to the corresponding nerves during surgery can cause persistent impotence that cannot be corrected with medication, so surgeons try to preserve the nerve endings in the surgical area.
Erectile dysfunction accompanies prostatectomy and can persist for up to two years, and in the case of complete transection of the nerves, the erection is disrupted forever. If the innervation of the pelvis is maintained, the erection is restored within this period, sex is possible after one and a half to two months, and to improve its quality, appropriate medications can be prescribed, for example, Viagra, Cialis.
Rehabilitation takes about one and a half months, during which the patient must follow certain rules regarding lifestyle and nutrition, which the attending physician informs him about.
Already on the second day you need to get up and walk; it is recommended to start eating after the first independent bowel movement. If bowel movements have not recovered by the third day, a cleansing enema is needed.
The diet has some peculiarities after prostatectomy. For three weeks you should avoid eating smoked foods, salty and fried foods, carbonated drinks and, of course, alcohol. The volume of liquid (juice, fruit drink, compote, water or tea) should be about 2-3 liters, but if there are contraindications from the heart or kidneys, then the drinking regime is set individually.
To restore urination and erectile function, it is recommended to perform special exercises to strengthen the muscles of the pelvic floor. These exercises can be obtained from your doctor or rehabilitation specialist. Physiotherapy procedures aimed at preventing inflammatory processes and increasing muscle tone are also possible.
For the first three months after the intervention, heavy lifting and heavy physical labor should be avoided, but you should not limit yourself to walking. It is recommended to wear a special bandage or tight swimming trunks to prevent postoperative swelling and lymph stagnation, especially pronounced after excision of the pelvic lymph nodes.
Reviews from patients who have undergone prostatectomy directly depend on the type of operation. The qualifications of the doctor and the level of the hospital play a significant role. After laparoscopy, the impressions are most positive, which is facilitated by early recovery, and during abdominal operations, possible complications can significantly slow down recovery.
Video: surgery – prostatectomy 1.5 months ago – patient review
Surgery to remove the prostate gland can be performed free of charge or for a fee. In the case of cancer and other severe lesions, treatment is carried out by surgeons and oncologists; hospitalization in a public hospital does not require any costs from the patient and is fully covered by insurance.
If the patient wants to undergo paid treatment, then he should be prepared for the costs. So, an operation in a public clinic will cost 50-70 thousand, and in a private clinic its cost reaches 100-150 thousand rubles.
In addition to paying for the operation itself, which is high-tech and therefore cannot be cheap, treatment on a commercial basis requires the cost of examinations and consultations, and also pays for days spent in the hospital.
Video: types of surgical operations for prostate cancer
Source: https://operaciya.info/urologia/prostatektomiya/
Prostatitis and surgery: surgical treatment, removal of the prostate, consequences
Prostatitis is an infection or inflammation of the prostate gland and is the most common problem in men under 50 years of age.
To treat the disease, in addition to the use of medications, traditional medicine and lifestyle changes, surgical intervention (operation) is often required.
Prostatitis and surgery - let’s take a closer look at surgical methods and their features.
Hide content
Indications and contraindications
Some groups of patients do not respond to drug treatment. One of these groups is patients with chronic prostatitis and chronic pelvic pain syndrome .
In addition to the usual symptoms, they experience depression, fatigue, weakness, malaise, irritable bowel syndrome and cognitive impairment.
For such patients, surgery is necessary to relieve these symptoms.
Indications for surgical intervention include:
- Urinary retention , accompanied by severe pain. Sometimes the pain is so severe that the patient cannot take urine tests; urine accumulates, causing pain in the lower abdomen and inability to urinate;
- Urinary tract infections (permanent/recurrent). Rarely, surgery is necessary to treat chronic bacterial prostatitis that does not respond to long-term antibiotic treatment. Surgery may be performed to eliminate infected areas of the prostate;
- Significant hemorrhage , recurrent hematuria;
- Prostate abscess . If antibiotics are not effective in treating the infection, the patient develops a prostate abscess. In this case, its drainage is necessary;
- Surgery is indicated for prostate cancer .
Surgery for prostatitis in men is not a common treatment method. Contacting specialists is a necessary measure (malignant formations).
Any method of surgical treatment of prostatitis has contraindications and consequences . Let's list them:
- Surgery is most often contraindicated in patients with acute bacterial prostatitis due to the possibility of systemic infection, although placement of a small drainage catheter is safe;
- Transurethral resection of prostate abscess is not recommended for patients with acute bacterial prostatitis, the incision may lead to impotence due to nerve damage, resection may affect the spread of bacteria, leading to sepsis;
- In patients with acute urinary retention, insertion of a catheter can cause severe discomfort;
- Laser treatment of prostatitis is not performed on patients with prostate cancer;
- Surgery is contraindicated in patients with cardiovascular disease , as well as in persons who have recently suffered a myocardial infarction ;
- The operation is not performed against the background of low platelets, renal failure, abdominal or thoracic aortic aneurysm, cystitis, pyelonephritis, or the presence of blood clots in the legs/lungs.
Kinds
Prostatectomy
Prostatectomy is a surgical treatment for localized prostate cancer, often performed in combination with radiation/chemotherapy and involves a series of procedures to remove part or all of the gland. There are different types of prostatectomy:
Radical prostatectomy is surgery to remove the entire prostate and lymph nodes. Surgery is indicated for the treatment of localized prostate cancer. Radical prostatectomy is also divided into several types:
- Robotic radical prostatectomy . The surgeon makes several small incisions in the lower abdomen to remove the prostate. The specialist sits on a special console and uses tools attached to a mechanical device (robot). The robotic approach is a more accurate and nerve-saving method that does not affect the quality of sexual life;
- Open radical prostatectomy . The surgeon makes an incision in the lower abdomen (retropubic surgery);
- Laparoscopic radical prostatectomy . The surgeon places a video camera and other instruments in the incision area to remove the prostate.
Open prostatectomy is indicated for patients with severe symptoms and severe enlargement of the prostate.
All types of prostatectomy are performed under general anesthesia or spinal anesthesia, which means the patient is conscious but not in pain. The duration of the procedure is 2-3 hours. Recovery time is from 4 to 6 weeks. The hospital stay is 1-3 days.
Most men need a urinary catheter for 5-10 days. Resumption of sexual activity is possible after 6-8 weeks.
Less than 10% of men experience complications after prostatectomy, and they are usually treatable and short-lived.
Prostate resection
Transurethral resection of the prostate (TURP) is a surgical procedure used to relieve symptoms of an enlarged prostate.
During TURP, a special instrument (resectoscope) is placed into the urethra. With its help, the surgeon trims tissue around the prostate that blocks urine, thereby increasing the size of the urethra.
Resection can be performed to prevent complications:
- Cystitis;
- Impaired kidney function;
- Incontinence;
- Urolithiasis disease;
- Hematuria.
The duration of the operation is from 60 to 90 minutes, general anesthesia . The hospital stay is 1-2 days. Most patients require a catheter within 4-7 days. Pain when urinating goes away within 1-4 weeks.
The recovery period is about 4-6 weeks; sexual activity can be resumed after 5-6 weeks.
After resection, most men experience significant relief of symptoms. Most patients do not experience relapses for 7-15 years.
Abscess drainage
Prostate abscess is a rare complication and quite often diagnosis is delayed due to the fact that the abscess mimics symptoms of urinary tract diseases. To treat a prostate abscess (and accumulation of pus), a drainage method .
The procedure is carried out using ultrasound and a special puncture needle, which is inserted into the prostate gland by puncture of the lower abdomen. First, an index finger is inserted into the rectum to determine the area of the prostate. The contents of the cavity filled with pus are sucked out with special instruments and washed with antiseptic agents, then the cavity is drained with rubber tubes.
Small abscesses are opened using the puncture method, large abscesses (more than 6 mm of pus) are opened using perineal access, and the abscess is drained directly through the rectum.
The procedure is performed under general anesthesia and lasts 60-90 minutes. The drainage remains in the cavity for 48-72 hours after surgery. Recovery time is 3-4 weeks.
Important. The consequences of opening an abscess include impotence, infertility . In some patients, the disease often progresses to a chronic stage. Abscess drainage is indicated for patients in whom the risk of abscess rupture is higher than the likelihood of subsequent complications.
Treatment of prostatitis with laser
Laser surgery is a minimally invasive method used to eliminate symptoms caused by an enlarged gland. The surgeon places a “sphere” (laser instrument) into the urethra (without making an incision). The laser removes excess tissue blocking the urethra by:
- Ablations. The laser burns excess tissue;
- Enucleation. The laser cuts the tissue.
Types of laser treatments:
- Photoselective vaporization . Excess tissue is evaporated by laser action;
- Holmium laser ablation . Similar procedure, uses a different type of laser;
- Holmium laser enucleation . The operation uses an instrument called a morcellator, which crushes the prostate tissue into small pieces, which are then easily removed.
Laser surgery has a number of advantages:
- Low likelihood of bleeding . The procedure is suitable for patients with blood clotting problems;
- No need to stay in the clinic after surgery. Laser surgery can be performed on an outpatient basis ;
- Fast recovery – about a week;
- No need to install a catheter. Although sometimes catheter placement is required for up to 24 hours;
- Efficiency . Improvements are noticeable immediately;
- No relapses . Laser surgery permanently eliminates urinary problems, since the removed tissue cannot regrow;
- There are no side effects (sometimes there is incontinence, blood in the urine, burning when urinating), side symptoms disappear within a few days.
Attention! Unfortunately, the laser method is not suitable for the treatment of malignant neoplasms of the prostate gland.
Laparoscopy
The operation is performed using special microchambers placed inside the abdominal cavity through small holes. Laparoscopic surgery eliminates the need for a large incision, so the risk of infection is minimized.
The recovery period is 4-6 weeks, the period in the hospital is up to a week (usually 3-4 days). The method is used to remove malignant tumors of the prostate gland that have not spread beyond its borders.
The main side effects after surgery include erection problems and urinary incontinence . The advantages are the absence of bleeding, the non-invasiveness of the method, and minimal damage to nearby tissues. After the procedure, the patient is fitted with a urinary catheter for up to 3 days.
Consequences and relapses
We list some of the negative consequences of surgical intervention in the treatment of prostatitis, including removal of the prostate in men:
- Severe bleeding is a rare but possible effect. Some patients lose large amounts of blood during surgery, although laser surgery and laparoscopy are exceptions;
- Temporary difficulty urinating . In this case, urinary catheters are used;
- Urinary tract infections are a rare but possible complication. Infection most often develops at the site of the catheter, in which case antibiotics are required; Incontinence;
- “Dry” orgasm . Surgery can provoke retrograde (reverse) ejaculation, which means that the sperm released during ejaculation enters the bladder without leaving the penis. Retrograde ejaculation is not a harmful or dangerous condition and does not affect the quality of sexual life. This long-term side effect occurs in approximately 75% of men who undergo prostate surgery and is most often a side symptom of TURP;
- erectile disfunction;
- Lymphedema - soft tissue swelling - is a rare but possible complication after removal of lymph nodes around the prostate;
- A change in the length of the penis is a possible effect after surgery associated with shortening the urethra, when part of it is removed along with the prostate;
- Inguinal hernia – performing a prostatectomy increases the chances of developing the disease in the future.
Need for re-treatment
Relapses most often occur after prostatectomy and drainage of abscesses, less often after resection of the prostate or laser method (extremely rare). In some cases, treatment is required because there is a narrowing (stricture) of the urethra or bladder neck.
Each method has its own advantages and disadvantages. The choice of surgical intervention method depends on the symptoms of the disease, the general health of the patient, and the response to drug treatment; the decision is made only by the attending physician.
In most cases, surgery has a beneficial effect on the course of the disease and eliminates its symptoms.
Video describing the operation
Source: https://LechenieBolezney.com/urology/prostatitis/lechenie/medicamentoznoe/hirurgicheskoe-vmeshatelstvo.html
Consequences of prostate removal in men
Removal of the prostate gland helps to cope with cancer at an advanced stage. Surgery is a last resort, which is used only in cases where none of the treatment options has brought the expected benefit. Surgical intervention directly depends on the stage of the disease. The prostate is removed completely or partially.
Appointment for surgery
Diseases of the prostate gland are common, as it is one of the most vulnerable places in a man’s body. In the early stages, they respond well to drug treatment, but there are cases when surgery is the only option. After examination and diagnosis, the doctor gives an opinion on the advisability of the procedure. Prescription for surgery:
- diagnosis of cancer at an advanced stage;
- prostate adenoma and its complications;
- the presence of a large amount of blood in the urine (hematuria);
- urolithiasis of the bladder;
- acute renal failure;
- retention of urine in the bladder and inability to urinate normally;
- serious diseases of the genitourinary system of an infectious nature.
- part of the organ protrudes (large diverticulum);
- absence of leukocytes in urine;
- prostatitis in the acute stage, especially if there are abscesses or phlegmons in the pelvic cavity.
It is very difficult for men to accept the fact that they will undergo surgery to remove their prostate. This is due to the fear of being childless and the inability to live a full sex life. This is far from true.
Only 25% of the consequences of prostate removal end sadly. This is not connected with the operation itself, but with the stage at which the intervention was carried out, and whether there were any negative complications after it.
For the most part, the operations are successful and the patient’s quality of life does not suffer.
Types of surgery
There are several techniques for removing the prostate gland. The choice of any of them depends on the stage of organ damage, as well as on whether the removal will be complete or partial.
Carrying out laser resection
This is one of the most modern methods of prostate removal. It has become widespread because it is safe and effective. Advantages of the procedure:
- After such an intervention, the likelihood of impotence is eliminated.
- The patient’s well-being improves within a few days after the operation to remove the prostate gland.
- Short hospital stay after surgery and short rehabilitation period.
- Long-term use of a catheter is not required - just one day is enough.
- The risk of bleeding after surgery is minimal, even in patients with poor blood clotting.
- No postoperative scars.
- This intervention is prescribed to patients with diabetes and high blood pressure.
Important. The big disadvantage is the price and lack of necessary equipment in many clinics.
This operation allows you to avoid postoperative complications such as blockage of the urethra as a result of the formation of blood clots and incomplete emptying of the bladder.
Laser resection is indicated for benign tumors in the prostate.
How is the incision procedure performed?
Such an intervention is already a dissection of organ tissue. With its help, expansion of the urethra is achieved to prevent its compression. The gland itself is not removed during the operation, but an incision is made on its surface.
This method of intervention is prescribed for:
- inflammation of the urinary tract;
- disruption of urine outflow;
- in case of frequent urge to urinate;
- residual urine after emptying the bladder.
After such an operation, retrograde ejaculation may occur. This means that when semen is released, it travels through the urethra into the bladder. The difficulty is that this condition can lead to childlessness.
Resection using the transurethral method
This is a partial excision of prostate tissue, performed through the urethra laparoscopically. It is indicated for benign growths of the prostate. Indications for the procedure:
- previous operations on the pelvic organs;
- with the simultaneous presence of adenoma and chronic prostatitis;
- if the patient is overweight, has heart problems;
- suspicion of a malignant tumor of the prostate gland in cancer;
- when the patient is young and it is very important to maintain his sexual function in a normal state;
- when the prostate volume is less than 80 cm3.
Radical prostatectomy
This operation is performed for malignant tumors, when the affected organ is excised along with the lymph nodes. This is an open operation and its implementation can have various negative consequences. Indications for such intervention:
- Cancer of stages 1 and 2, which has not spread to neighboring organs and tissues, without metastasis.
- Prostate adenoma in the very last stages, when there is no response to other types of treatment.
- Stage 3 cancer, when the outflow of urine is very difficult.
Risk of bleeding
Bleeding is a very common complication after prostate surgery. It is observed in approximately two and a half cases. Such postoperative bleeding causes large blood loss and blockage of the urethra with blood clots. In cases of heavy blood loss, blood transfusion is indicated.
Important. This type of complication occurs after radical prostatectomy or transurethral resection.
Water intoxication
An equally frequent and severe postoperative complication. It occurs when fluid used during surgery to irrigate the urethra enters the bloodstream. According to statistics, such a complication has a probability of 0.1-6.7%. To minimize such consequences after removal of the prostate gland, modern solutions are used.
Severe urinary retention
A typical complication after prostate resection. It occurs as a result of blockage of the urethra by blood clots, the physiology of the muscular system of the bladder, or an error made by the doctor during the operation. The consequences are the most severe, but there are measures to prevent them.
Incontinence occurs in 1-2% of cases and is either permanent or occurs during intense physical exertion. If everything is fine after the procedure, this condition goes away after 5-6 days. In rare cases, auxiliary therapy is used.
Urine leakage
The probability of this condition is 2-10%. Urine is spontaneously released in a variety of circumstances, accompanied by pain and difficulty in flowing out. Such a complication, if it does not go away in the shortest possible time, may be due to insufficient excision of gland tissue during the operation. In these cases, repeated intervention is prescribed.
Inflammatory processes
This type of complication can occur after any surgical intervention on the prostate gland. The likelihood of inflammation is in every 5th surgical procedure.
Signs become obvious within a few days after surgery or after several days of bladder catheterization. Antibiotics are prescribed to relieve such conditions.
The complication sometimes becomes chronic.
Lack of ejaculation after orgasm
This pathology is called retrograde ejaculation. In this case, the seminal fluid not only does not come out, but also enters the bladder. This condition occurs in almost 99%. If retrograde ejaculation is complete, then there will be no sperm during orgasm.
If it is partial, then, when examining a urine test, the presence of seminal fluid can be detected in it. This is not dangerous for the body, since, in any case, sperm will be released along with urine.
However, in terms of conceiving a child, this consequence of removal in a man can cause infertility.
Problems with potency
This is exactly what men fear most in the postoperative period. This pathology occurs in 4-10% of cases.
Other reasons
- There is pain in the suture area after surgery.
- Presence of blood in the urine. This is due to the loss of the formed scab or the features of the function that maintains the liquid state of the blood (hemostasis).
- Severe pain in the lower abdomen.
- Suture infection (in the late postoperative period, this complication is associated with violation of hygiene rules).
- Inability to achieve orgasm, as well as painful sensations during sexual intercourse.
Recovery period
For the early recovery period (5-7 days after the intervention), the most important thing is to normalize urination. The recovery period itself may take several months. This largely depends on the age group of the patient.
Methods to speed up health recovery:
- Strengthen the pelvic muscles with special exercises. Kegel exercises quickly normalize the urination process.
- Massage and vibration therapy procedures.
- Use of special devices: vacuum erector and electrical stimulator.
- During this time, you should avoid lifting loads weighing more than 3 kg.
- It is not recommended to spend long periods of time sitting or driving a vehicle. Moderate physical activity is beneficial.
- For the first two months you need to abstain from sexual contact, and three months after the operation you can resume sexual activity - this is also an important stage in normal recovery. The psycho-emotional attitude is very important here: even if at first everything turns out completely differently than before the operation, it is important to be patient and realize that over time everything will return to normal. If problems with potency were observed before the intervention, they may worsen after the operation.
- It is important to follow a special diet and avoid smoked, spicy and salty foods and foods.
- Take antibacterial treatment for the prescribed time.
- Quit smoking and don't drink alcohol. Such habits are contraindicated in case of complications on the prostate gland.
Source: https://myzhelezy.ru/smeshannoj-sekretsii/polovye/posledstviya-udaleniya-predstatelnoj.html
Removal of the prostate: indications and methods of surgery
- Performed as a last resort to cure chronic prostatitis (partial resection) or prostate cancer (radical resection).
- It is an invasive abdominal procedure that can be performed with a single incision in the lower abdomen, perineum, or a series of small incisions.
- Removing the prostate often entails problems such as:
- erectile dysfunction (difficulty achieving an erection);
- lack of ejaculation;
- urinary incontinence;
- dysuria (difficulty urinating);
- infections, and not only in the operated area, since the body will be greatly weakened;
- severe pain in the first weeks after surgery.
The recovery period can take a year, or sometimes longer.
Indications for prostate removal
Indications for complete removal of the prostate are:
- a cancer tumor localized within the prostate gland;
- advanced case of prostate adenoma (radical adenomectomy);
- the presence of a large number of stones in the prostate;
- a fast-growing tumor, also known as a high-grade tumor in a young man.
For older people with slow-growing prostate cancer, removal of the prostate may not be necessary. This is because the cancer can grow so slowly that a person is more likely to die of old age or other causes than from prostate cancer. Also, for the non-surgical treatment of prostate cancer, men of all ages can be prescribed Xtandi, Zytiga or Estracite.
Prostate cancer may be indicated by an increase in the level of PSA, an antigen produced by the prostate, to 4-10 ng/ml.
Prostate surgery (the technical term is prostatectomy) will only help those patients whose tumor is limited to the prostate gland. The oldest type of prostate removal surgery, open prostatectomy, involves complete removal of the entire gland and possibly the seminal vesicles and surrounding nerves and veins.
The part of the urethra that passes through the prostate area is also removed. This helps prevent relapse of the disease, but entails a lot of potential complications. A more gentle surgical option is nerve-sparing prostatectomy.
This type of surgery is intended for early diagnosis of prostate cancer, which is located inside the prostate. The cancer must be far from the two bundles of nerves that control erections.
The purpose of the surgery is to reduce the risk of erection problems after surgery. The surgeon cuts the prostate tissue without damaging the nerve bundles.
However, he will have to remove them if the cancer is close to or already in the nerves.
Cancer will not be cured if the surgeon leaves the tumor in an attempt to save the nerves. If the cancer is only on one side of the prostate, the surgeon may leave the other side of the prostate intact and prescribe the drug Avastin. However, the patient will still experience difficulties with erection, although not as significant as with radical prostatectomy.
There are several types of prostate surgery: retropubic, perineal, laparoscopic and robotic.
They are classified depending on the location of the incision:
- The retroplated prostate removal method involves making an incision in the lower abdomen, from the navel to the pubic bone. The incision is 8 to 10 centimeters in length. This method is more nerve-saving compared to the perineal method.
- The perineal method involves a four-centimeter incision in the perineum, which involves the muscles and tissue between the scrotum and anal sphincter. It is performed faster and with less blood loss than the retropubic one, but more often leads to nerve damage and, as a result, impotence.
- Laparoscopic and robotic methods. A laparoscope is a thin, tube-based instrument that allows the surgeon to see inside the abdomen and remove the prostate through a series of small incisions rather than one long one. The robotic procedure uses the same incisions and instruments as the laparoscopic procedure, but the surgeon uses robotic arms to perform the operation remotely. In terms of benefit to the patient, these two methods of prostate removal are almost identical. The price of a laparoscopic procedure varies from 70,000 to 100,000 rubles, while a robotic procedure costs up to 350,000 rubles.
When there is a slight growth of prostate tissue, and, in rare cases, when there is a cancerous tumor in the prostate with obstruction of the urinary tract, not the entire prostate is removed, but only part of it.
This endoscopic operation is called “transurethral resection of the prostate,” abbreviated as TUR. Using a resectoscope inserted through the urethra into the bladder, the altered tissue is removed without affecting the healthy tissue of the gland. A modern, but expensive option for TUR is coagulation of the affected prostate tissue with a laser.
Bleeding
Radical prostatectomy, the traditional procedure for treating prostate cancer, has always been associated with bleeding.
As the procedure has improved, blood loss has been reduced, but it is still significant. On average, surgery to remove the prostate results in the loss of about 500-900 ml of blood.
While young, healthy people can usually tolerate this amount of blood loss without any adverse effects, older and/or sick people cannot tolerate large amounts of blood loss without harming their health.
As a result, most men donate blood for several weeks before surgery, and it is transfused back to them during surgery.
Robotic surgery, unlike radical prostatectomy, results in significantly less bleeding (about 100-200 milliliters).
This difference is because robotic surgery involves a process called insufflation, in which gas is pumped into the abdominal cavity.
It creates pressure that stops bleeding from veins that would otherwise bleed freely during traditional surgery.
Therefore, many surgeons performing robotic prostatectomy do not ask patients to donate blood before the procedure.
TUR syndrome is a very rare phenomenon (according to statistics, it occurs in 0.1-1% of cases), in which a large amount of irrigation fluid enters the bloodstream. As a result, so-called “water intoxication” occurs, characterized by an increase in the volume of extracellular fluid, hypervolemia, a decrease in the amount of blood electrolytes and sometimes damage to red blood cells.
Incontinence is a common problem for men after prostate surgery. It usually occurs after the catheter is removed. Typically, urinary incontinence occurs when pressure on the bladder increases, such as from sneezing, coughing, or lifting heavy objects. One month after surgery, cases of urinary incontinence become less common.
After a year, only a small percentage of men complain about this problem. Kegel exercises, which are performed to strengthen the pelvic floor muscles, will help solve it. You should also urinate before going to bed at night.
Retrograde ejaculation
Even for those people who regain full erections after surgery, sex will never be the same.
The prostate and seminal vesicles produce most of the seminal fluid that men ejaculate when they reach orgasm.
During prostate removal surgery, both the prostate gland and the seminal vesicles are removed and their connection to the testicles is severed (as with a vasectomy).
As a result, when a man reaches orgasm, he experiences “dry” ejaculation. While the operated person still feels pleasure after sex, it feels a little different. Due to the fact that sperm does not appear during orgasm, men are infertile after prostatectomy.
The risk of erectile dysfunction and impotence remains a serious concern after prostate surgery. This is probably the main reason for men's fear of this procedure.
The occurrence of impotence after prostate surgery is largely determined by the age of the patient and his sexual potency before prostatectomy. Many men regain their ability to have spontaneous erections without assistance, but it may take time (about a year after surgery) before erections return.
Doctors may prescribe medications such as sildenafil to stimulate erections and normalize intimate life.
Proper nutrition also plays an important role, including foods with selenium, zinc and polyunsaturated fatty acids.
In particularly severe cases, your doctor may recommend installing a corpora cavernosa implant. Robotic procedures have a lower risk of long-term impotence.
Inflammatory diseases
Surgery to remove the prostate is rarely associated with infection. With adequate antibiotic therapy, most patients successfully avoid inflammatory diseases in the postoperative period.
However, if an infection does occur, the site of its origin is the incision, the edges of which turn red, become hot to the touch, and sometimes pus flows from the incision. An infection can also occur in the bladder.
Both of these types of infections can be successfully treated with antibiotics. Iskador is also often appointed.
Patients should keep the incision site clean by using a solution of hydrogen peroxide and water. Patients should clean the penis and anus several times a day, especially after bowel movements, with soap and water.
Source: https://med88.ru/lechenie-prostatita/udalenie-prostaty/
Prostate surgery: in what cases and how is prostate surgery performed?
Prostate diseases, previously considered age-related pathologies, are now diagnosed in 35-40 year old men.
Despite the efforts of specialists, it is not always possible to manage with conservative treatment methods; 30% of patients require surgical intervention.
And prostate surgery, according to statistics, firmly holds 2nd place in urology. Let's consider what types of surgical intervention there are and what indications exist for them.
Indications for surgical treatment methods
Surgery on the prostate gland often becomes the only possible method for a man to get rid of painful spasms when urinating, as well as eliminate the growth of the tumor.
Prostate surgery is performed in the following cases:
- Prostate tissue growth – prostate adenoma.
- Purulent prostatitis or abscesses in the body of the prostate gland.
- Narrowing of the urethra (urethra).
- Delay or absence of urination.
- Prostate tumors – both benign and malignant.
- Bloody discharge from the urethra.
- Rapid proliferation of connective tissue – sclerosis or fibrosis of the prostate.
- Urinary incontinence.
Urologists or andrologists are the names of specialists who should be contacted if alarming symptoms appear. At the same time, urologists deal with pathologies of the urinary system as a whole, while andrologists study disorders of the male reproductive system. But a doctor of both first and second specialization, after all examinations, can recommend prostate surgery.
Note! Prostate surgery is performed strictly in a hospital setting by surgeons under anesthesia.
Surgery on the prostate gland is performed in a hospital setting
What types of operations are there?
The types of operations depend on the degree of prostate damage. In case of voluminous tumors (more than 80 mm), the presence of multiple stones in the urinary system, developed diverticulosis of the bladder membranes, preference is given to a radical method - surgery to remove prostate growth or adenomectomy.
If the tumor size is less than 80 ml, a more gentle operation on the prostate is performed - excision of the adenoma. With mild inflammation and a small adenoma, surgeons tend to use low-traumatic endoscopic methods.
Regardless of what type of prostate surgery is planned, there are a number of contraindications to surgery:
- Severe forms of cardiac, renal and pulmonary failure (there is a risk of intolerance to general anesthesia).
- Cystitis, pyelonephritis in the acute stage.
- Infectious diseases.
- Serious pathologies of the cardiovascular system and brain.
Depending on the degree of intervention and penetration into the affected area, there are several methods for surgical tumor removal.
The operation varies in form of intervention
Open or traditional surgery
Operations to remove glandular growths of the prostate, carried out in the traditional open way, 30 years ago were practically no alternative method of tumor removal.
Currently, other methods are widely practiced, but open adenomectomy has not lost its relevance as a way to cope with large tumors and prevent the degeneration of a benign tumor into a malignant one.
The operation is also indicated for significant accumulation of stones and proliferation of diverticula in the urinary system.
The operation is classified as abdominal, since the intervention occurs through an open bladder under general anesthesia.
To predict possible complications and recovery time before surgery, general and biochemical blood and urine tests, a blood test for AIDS and sexually transmitted diseases are required. The list of preliminary preparation also includes an ECG and ultrasound of the abdominal organs.
The course of the operation, which requires certain skills and qualifications of the surgeon, includes a number of stages:
- After the necessary hygienic procedures, a longitudinal or transverse incision is made in the abdomen, penetrating through the dermis and subcutaneous fat tissue.
- Dissection of the anterior wall of the bladder allows the contents of the bladder to be analyzed for the presence of stones and diverticula.
- The third most crucial moment of the operation is palpation of the detected tumor and its isolation.
- Penetrating into the internal opening of the urethra, the surgeon uses his index finger to remove tissue growth that interferes with the normal functioning of the gland itself.
- After the tumor is isolated, it is carefully removed through the opened organ, being careful not to damage adjacent structures. The excised tumor is certainly sent for histological examination.
Like any type of surgical activity, open surgery has undeniable advantages, but also has its disadvantages.
The main advantage of the traditional open method is radicalism, that is, the final and irreversible cutting off of the tumor with all aggravating symptoms.
The main negative consequence of the method is the likelihood of bleeding in the initial postoperative period. The danger is not so much blood loss as the possible blocking of the outlet hole in the bladder by a blood clot. To prevent this situation, the organ is washed with sterile saline through a catheter.
Getting rid of a tumor also has its price - the consequences of anesthesia, a long recovery period (up to 3 months), the risks of complications (suppuration and bleeding of the wound, the formation of fistulas). The postoperative suture does not paint either.
Source: https://prostatu.guru/lechenie/kak-delayut-operatsiyu-na-prostate.html