Home › Autoimmune diseases ›
Autoimmune diseases are pathologies that occur when the body's defenses malfunction. Women are more likely to experience such diseases than men.
What is it and the reasons for its development
Autoimmune pathologies occur due to disorders in the body, which can be triggered by a number of factors. Most often, it is based on a hereditary predisposition. Immune cells, instead of foreign agents, begin to attack the tissues of various organs. Often this pathological process occurs in the thyroid gland and joints.
The necessary substances do not have time to replenish the losses received from the destructive effects of one’s own immune system. Such disorders in the body can be provoked by:
- harmful working conditions;
- viral and bacterial infections;
- genetic mutations during fetal development.
Main symptoms
Autoimmune processes in the body manifest themselves in the form of:
- hair loss;
- inflammatory process in joints, gastrointestinal tract and thyroid gland;
- arterial thrombosis;
- numerous miscarriages;
- joint pain;
- weaknesses;
- skin itching;
- enlargement of the affected organ;
- menstrual irregularities;
- abdominal pain;
- digestive disorders;
- deterioration of general condition;
- weight changes;
- urinary disorders;
- trophic ulcers;
- increased appetite;
- mood changes;
- mental disorders;
- convulsions and trembling of limbs.
Autoimmune disorders provoke pallor, allergic reactions to cold, as well as cardiovascular pathologies.
List of diseases
The most common autoimmune diseases, the causes of which are similar:
- Alopecia areata - baldness occurs as the immune system attacks the hair follicles.
- Autoimmune hepatitis - inflammation of the liver occurs, as its cells come under the aggressive influence of T-lymphocytes. The skin color changes to yellow, and the causative organ increases in size.
- Celiac disease is gluten intolerance. At the same time, the body responds to the consumption of cereals with a violent reaction in the form of nausea, vomiting, diarrhea, flatulence and stomach pain.
- Type 1 diabetes - the immune system attacks the cells that produce insulin. With the development of this disease, a person is constantly accompanied by thirst, increased fatigue, blurred vision, etc.
- Graves' disease is accompanied by increased production of thyroid hormones by the thyroid gland. In this case, symptoms such as emotional instability, hand tremors, insomnia, and disruptions in the menstrual cycle occur. An increase in body temperature and a decrease in body weight may occur.
- Hashimoto's disease develops as a result of decreased production of thyroid hormones. In this case, the person is accompanied by constant fatigue, constipation, sensitivity to low temperatures, etc.
- Julian-Barre syndrome - manifests itself in the form of damage to the nerve bundle connecting the spinal cord and brain. As the disease progresses, paralysis may develop.
- Hemolytic anemia - the immune system destroys red blood cells, causing tissues to suffer from hypoxia.
- Idiopathic purpura - platelets are destroyed, resulting in impaired blood clotting ability. There is an increased risk of bleeding, prolonged and heavy menstruation and bruises.
- Inflammatory bowel disease is Crohn's disease or ulcerative colitis. Immune cells attack the mucous membrane, causing an ulcer, which occurs with bleeding, pain, weight loss and other disorders.
- Inflammatory myopathy - damage to the muscular system occurs. The person experiences weakness and feels unsatisfactory.
- Multiple sclerosis - your own immune cells attack the nerve sheath. In this case, coordination of movements is impaired, and problems with speech may arise.
- Biliary cirrhosis - the liver and bile ducts are destroyed. A yellow tint to the skin, itching, nausea and other digestive disorders appear.
- Myasthenia gravis - the affected area includes nerves and muscles. A person constantly feels weak, any movement is difficult.
- Psoriasis - destruction of skin cells occurs, as a result, the layers of the epidermis are distributed incorrectly.
- Rheumatoid arthritis is a systemic autoimmune disease. The body's defenses attack the lining of the joints. The disease is accompanied by discomfort during movement and inflammatory processes.
- Scleroderma is a pathological growth of connective tissue.
- Vitiligo - cells that produce melanin are destroyed. In this case, the skin is colored unevenly.
- Systemic lupus erythematosus - the affected area includes the joints, heart, lungs, skin and kidneys. The disease is extremely difficult.
- Sjögren's syndrome - the salivary and lacrimal glands are affected by the immune system.
- Antiphospholipid syndrome - the lining of blood vessels, veins and arteries is damaged.
How does autoimmune thyroiditis manifest and how to treat it?
Which doctor can diagnose
An immunologist is a doctor who specializes in the treatment of such pathologies. The specialist takes into account the patient’s blood test, which confirms or refutes the alleged diagnosis. Additionally, consultations may be required:
- urologist;
- therapist;
- rheumatologist;
- endocrinologist;
- dermatologist;
- neurologist;
- hematologist;
- gastroenterologist.
Basic treatment methods
Treatment of autoimmune pathologies is aimed at alleviating the symptoms of the disease. For this purpose, painkillers are often prescribed, such as: Ibuprofen, Analgin, Spazmalgon, etc.
An important stage in treatment is to compensate for the deficiency of essential substances that should be produced normally.
For example, in case of diabetes mellitus, insulin injections are prescribed, and in case of decreased thyroid function, appropriate hormones are prescribed.
The main thing in the treatment of these types of diseases is suppression of immune activity. This is necessary to ensure that the protective cells do not completely destroy the organ tissue and provoke life-threatening complications.
In this case, immunosuppressants suppress the production of antibodies. Such drugs are prescribed only by a doctor, since if they are taken incorrectly, they can provoke a number of dangerous consequences, including the addition of an infection.
Prevention
In order to reduce the risk of autoimmune diseases, it is necessary to lead a healthy lifestyle and give up bad habits. It is important not to take any strong medications without a doctor’s prescription. It is necessary to reduce the amount of stress, relax more often and spend time in the fresh air.
Nutrition plays a crucial role in prevention. It is recommended to eat more fresh fruits and vegetables, cereals and dairy products. It is necessary to abandon carcinogens, fats and GMOs.
Timely treatment of infectious and viral pathologies plays an important role. It is not recommended to start diseases and self-medicate. You should move more and avoid physical inactivity. If there is a genetic predisposition to autoimmune diseases, then it is important to visit an immunologist once a year and monitor the condition of the body.
How does autoimmune thyroiditis manifest and how to treat What are autoimmune diseases in simple words and a list of diseases Link to the main publication
Source: https://immunitet1.ru/autoimmunnye-zabolevaniya/spisok-boleznej
Features of scleritis and its dangerous consequences
Scleritis is an inflammatory process in the fibrous membrane of the eye or sclera. The outer fibrous membrane protects the eyeball. It is dense, so it can fix blood vessels, nerves and muscles. The sclera is also the framework for the inner membranes of the eye.
Structure of the sclera
The sclera consists of an outer mucosa (conjunctiva), an inner dense Tenon's membrane and an episclera.
The Tenon's membrane of the sclera consists mostly of collagen fibers, which is why the sclera is colored white. Under Tenon's layer is the episclera. This is a loose layer of blood vessels.
Under the sclera there is also a brown membrane. It smoothly passes into the choroid of the eye, having a loose structure.
The peculiarity of scleritis is that inflammation covers all layers of the sclera. The disease is dangerous because it can be mild and gradually lead to destruction of the structure of the sclera. This is fraught with complete delamination of the outer shell of the eyeball and damage to tissues that lie deeper. Such disorders can lead to vision loss.
Classification of violations
Severe but limited inflammation is called nodular, and widespread scleritis is considered diffuse. Sometimes necrotizing scleritis (perforating scleromalacia) is diagnosed.
Types of scleritis:
- The anterior one, which develops in the scleral membrane accessible to inspection.
- Posterior, which develops in the scleral membrane, inaccessible for inspection.
Causes of inflammation of the sclera
Most often, the disease is diagnosed in women 30-50 years old. Most patients also have connective tissue related diseases. With necrotizing scleritis, connective tissue diseases occur in 50% of patients, and in patients with nodular and diffuse scleritis in 20% of cases. Most often, scleritis affects the anterior segments of the eye.
The disease can develop for many reasons. Previously, it was believed that the most common causes of inflammation of the sclera were sarcoidosis, tuberculosis and syphilis, but now streptococcal infections occupy the first place.
Often the disease is a symptom of pneumococcal pneumonia, inflammation of the paranasal sinuses, metabolic diseases (gout).
Endophthalmitis (accumulation of pus in the vitreous) and panophthalmitis (purulent inflammation of the entire eye) can cause scleritis as a secondary disorder.
Rheumatological disorders are considered the main cause of scleritis. The connection between scleritis, rheumatism and polyarthritis cannot be denied.
In infectious scleritis, the cause lies in a bacterial infection of the cornea. Most often, inflammation is the focus of activity of herpes zoster, Pseudomonas aeruginosa, Staph. aureus, Strept. pneumoniae. This disease is difficult to cure.
Sometimes the cause of inflammation of the sclera is mechanical or chemical injury. Inflammation may result from removal of a pterygium (a triangular defect of the eye near the palpebral fissure, which consists of diseased conjunctival tissue). Scleritis can also be diagnosed after treatment with ultraviolet beta radiation and mitomycin C.
The main causes of scleritis:
- In half of the cases, inflammation of the sclera is a sign of a systemic disease.
- Postsurgical scleritis is less commonly diagnosed, the cause of which is not fully understood. Six months after surgery, patients develop a focus of inflammation and necrosis. Inflammation of the sclera after surgery develops only in the area involved in the process.
- Infectious scleritis is a consequence of the spread of infection from a corneal ulcer.
Inflammation of the sclera can be a symptom of the following diseases:
- Wegener's granulomatosis;
- systemic lupus erythematosus;
- polyarteritis nodosa;
- recurrent arthritis;
- Bekhterev's disease;
- rheumatoid arthritis.
If scleritis is detected, you should consult a rheumatologist and immunologist. Sometimes the disease develops after surgery. Post-surgical scleritis can persist for up to six months after surgery.
Inflammation with scleritis develops in the same way as a bacterial allergy. It is believed that inflammation of the sclera may have an autoimmune basis, and therefore recurs very often.
Symptoms of scleritis
Symptoms of scleritis appear gradually. This usually takes several days. Almost always, inflammation provokes severe pain that spreads to the nearest areas of the head. Patients often describe the pain of scleritis as deep and boring. The intensity of the pain can interfere with sleep and appetite.
Symptoms of scleral inflammation:
- Scleritis is characterized by pain. With mild inflammation, discomfort appears, the pain is moderate and intermittent. With severe destruction of the sclera, the pain is regular, intense and shooting. Pain with severe inflammation can spread to the temple, jaw and eyebrow.
- With scleritis, severe redness of the eyeball is observed. The redness has a purple tint. Often the redness covers the entire cornea. This is due to the fact that the blood vessels dilate. Depending on the intensity of the inflammatory process, redness may be limited or extensive.
- Inflammation often provokes lacrimation. This occurs due to irritation of the nerves. Lacrimation increases with severe pain.
- Pale yellow spots on the sclera are a sign of necrosis or scleral separation. Often with hidden scleritis, spots are the only symptom, but the most critical.
- With scleritis, visual acuity decreases only with damage to the central zone of the retina and with retinal detachment. Vision also deteriorates when inflammation spreads to deeper tissues and when the sclera melts.
- Some patients develop photophobia.
- Spots of hyperemia (overflow of blood in the blood vessels of the eye) are located under the conjunctiva and have a purple color (by this criterion they are distinguished from spots with episcleritis). Hyperemia can be local and cover no more than one quadrant of the eye, or extensive, involving the entire eye. With extensive damage, edematous nodes or necrosis are sometimes detected.
- With strong infiltration (penetration of uncharacteristic particles into the tissue), necrosis and scarring begin in the affected areas, which gradually thin the sclera.
- After inflammation, grayish traces always remain, which indicate places where the sclera has thinned. Through these foci, pigments of the choroid and ciliary body can be seen.
- Sometimes protrusion of lesions on the sclera occurs. The phenomenon is called staphyloma. When protruding, vision deteriorates. Visual acuity also decreases when complicated by astigmatism and other changes in the stratum corneum and iris.
Scleritis of the posterior shell
Posterior scleritis is a fairly rare occurrence. The patient may complain of eye pain and tension. Sometimes there is limited mobility, retinal detachment, and swelling of the optic nerve.
With scleritis of the posterior layer, there may not be any pronounced symptoms. The inflammation will not be noticeable even when examining the eye. Posterior scleritis can be identified by swelling of the eyelid and retina and impaired functionality of the eye.
Scleritis of the posterior wall can be detected only with tomography and echography. Most often, the disease is a consequence of tuberculosis, herpes, rheumatism and syphilis. Often complicated by keratitis, iridocyclitis, cataracts and chronic increased intraocular pressure.
Necrotizing scleritis
With advanced necrotizing scleritis, perforation of the eye is observed. If a patient with necrotizing scleritis has a connective tissue disease, systemic vasculitis is most likely the cause of the inflammation. This form of scleritis is rare, but can occur without inflammation. It is then called perforating scleritis.
If there is no inflammation with necrotizing scleritis, it is worth checking the patient for rheumatoid arthritis. The absence of symptoms leads to a delay in treatment; the sclera becomes thinner and ruptures with any injury.
Diagnosis and treatment of scleritis
To recognize the disease, the doctor must analyze the patient’s complaints and examine the eyes. When treating scleral inflammation, local and general anti-inflammatory drugs are used. If there is a high probability of developing perforation, scleral transplantation is recommended.
For scleritis, primary therapy includes glucocorticosteroids. If the patient has a decreased response to glucocorticosteroids, necrotizing vasculitis or connective tissue disease is diagnosed, immunosuppressive drugs (azathioprine, cyclophosphamide) are required. These medications should be prescribed by a rheumatologist.
For local therapy, corticosteroids (maxidex, dexazone, hydrocortisone-POS, oftan-dexamethasone) and non-steroidal anti-inflammatory drugs (naklof, diclofenac, indomethacin) are used. Doctors will also prescribe cyclosporine. Cytostatics perfectly relieve the symptoms of the inflammatory process.
To treat necrotizing scleritis, as a symptom of a systemic disease, it is necessary to use immunosuppressants (cytophosphamide, corticosteroids, cyclosporine). When inflammation subsides, physiotherapy may be prescribed: electrophoresis, ultra-high frequency therapy, ultrasound therapy. Since scleritis is almost always a manifestation of another disease, it is necessary to treat the cause.
Surgery for scleritis
Surgical intervention for scleritis is indicated in cases of severe complications of the condition, when deformation of the deep layers of the sclera, cornea and iris occurs. Surgery is also necessary for an abscess.
If the thinning is severe, a donor sclera transplant is required. If the cornea is also affected (with a significant decrease in vision), its implantation is also necessary.
Complications of inflammation of the sclera
It often happens that inflammation of the sclera is complicated by the cornea, causing sclerosing keratitis or inflammation of the iris and ciliary body.
These complications are characterized by adhesions between the lens and the pupillary edge of the iris. Precipitates also form on the posterior wall of the cornea, and clouding of the anterior chamber of the eye is observed.
With scleritis, the conjunctiva connects to the affected area of the sclera, swelling occurs.
Complications of scleritis:
- keratitis and visual impairment when moving to the cornea;
- iridocyclitis when inflammation spreads to the iris and ciliary body;
- opacity in the vitreous body;
- thinning of scleral tissue, formation of protrusions and stretches;
- scarring, deformation of the eyeball;
- astigmatism;
- secondary glaucoma with involvement of Schlemm's canal and ciliary body;
- scleral abscess;
- swelling;
- retinal detachment;
- clouding of the cornea due to malnutrition;
- endophthalmitis (purulent inflammation of the inner membrane);
- panophthalmitis (purulent inflammation of the entire eye).
Forecast
With scleritis, 14% of patients experience pathological changes that provoke severe visual deterioration in the first year of the disease. In 30% of patients, vision declines within 3 years. With necrotizing scleritis caused by systemic vasculitis, 50% of patients die within 10 years, mainly from a heart attack.
Prevention
Inflammation of the sclera can be prevented by timely treatment of infection of any location, diagnosis of autoimmune disorders of an infectious nature and correction of metabolic disorders.
Source: https://BeregiZrenie.ru/vospaleniya/sklerit/
Autoimmune Diseases: When Defense Becomes the Enemy
A butterfly rash on the bridge of the nose and cheeks is a common symptom of systemic lupus erythematosus (SLE).
Autoimmune diseases are a group of diseases characterized by problems with the immune system, which produces autoantibodies that attack healthy tissue in the body. These diseases are more common in women than in men.
Contents:
There are at least 80 types of autoimmune diseases, and all of them are chronic. The exact etiology is unknown, however, a genetic predisposition has been proven. For example, systemic lupus erythematosus can often occur in several family members, suggesting a genetic basis.
Symptoms of autoimmune diseases
Although there are many different autoimmune diseases, many have similar symptoms, such as fatigue, dizziness and mild fever. Symptoms may come and go, and the severity of symptoms may vary from person to person.
Here is an example of more detailed symptoms for some autoimmune diseases:
- Systemic lupus erythematosus (SLE) - symptoms depend on which organs are affected. However, the hallmark sign of SLE is redness and a butterfly-shaped rash on the face. Other symptoms: weakness, pain in muscles and joints, fever.
- Rheumatoid arthritis - painful, swollen and deformed joints, decreased motor function. Fatigue, fever, weight loss, eye inflammation, lung disease, and anemia may also occur.
- Alopecia areata is characterized by patchy hair loss on the scalp, face, or other areas of the body.
- Antiphospholipid syndrome ( APS ) - blood clots in veins or arteries, multiple miscarriages; a lacy, mesh-like red rash on the wrists and knees; retardation in physical and mental development.
- Autoimmune hepatitis - fatigue, enlarged liver, yellowing of the skin or whites of the eyes, itchy skin, joint pain, abdominal pain.
- Celiac disease - gluten intolerance, abdominal bloating and pain, diarrhea or constipation, weight loss or gain, fatigue, missed periods, itchy skin rash, infertility or miscarriage.
- Vitiligo is white patches on areas exposed to the sun, as well as in the armpits and genitals. Hair turns gray early, loss of color in the mouth.
The sudden and severe onset of symptoms is called a flare, and their disappearance is called remission.
Vitiligo. White spots on the skin and gray hair
Who is at increased risk of getting sick?
Diseases in this group can occur in any person, however, some people have an increased risk of acquiring them.
Women's immune systems fail 9 times more often than men's.
- People who have relatives with a history of autoimmune diseases.
Inheriting certain genes can make you more likely to have an autoimmune disease, such as lupus or multiple sclerosis.
- People exposed to certain environmental conditions and substances.
Sunlight, chemicals called solvents, and bacterial and viral infections are associated with many autoimmune diseases. They may be the cause of some of them or aggravate their course (be a trigger for an outbreak).
- People of a particular race or ethnic origin.
Several autoimmune diseases are more common or more severe in certain groups of people. For example, type 1 diabetes is more common in white people. Lupus is most dangerous in African Americans and Hispanics.
Types of Autoimmune Diseases
Making an accurate diagnosis can be a difficult task for a doctor. Common diseases that are usually considered autoimmune include:
- Diabetes mellitus type 1
- Celiac disease
- Rheumatoid arthritis
- Inflammatory bowel disease
- Multiple sclerosis
- Psoriasis
- Graves' disease
- Systemic lupus erythematosus
- Sjögren's syndrome
- Crohn's disease
This list can be supplemented by systemic scleroderma, Behcet's syndrome, Hashimoto's thyroiditis, Heinz syndrome, psoriatic arthritis, glomerulonephritis, hidradenitis suppurativa and many others. Little is known about them and it is unclear how and where they came from, but the influence of genes and environmental factors has been proven.
Genetic predisposition
Autoimmune diseases are characterized by a multifactorial etiology.
Possession of certain genes significantly increases the risk of developing certain systemic diseases, but the main trigger is believed to be environmental factors that can influence these genes.
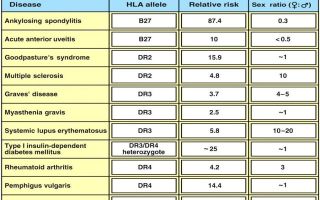
Human leukocyte antigens and susceptibility to autoimmune diseases
On the subject: Autoimmune diseases in women are 9 times more common than in men.
Impact of autoimmune diseases on pregnancy
Women with autoimmune diseases can have children. However, there may be certain risks for the mother or baby, depending on the disease and its severity.
For example, pregnant women with lupus have a higher risk of preterm birth and stillbirth. Women with myasthenia gravis may have symptoms that lead to breathing problems during pregnancy.
Additionally, some medications used to treat autoimmune diseases may not be safe for use during pregnancy.
If you want to have a child, it is best to discuss this with your doctor in advance. Your doctor may advise you to wait until your disease goes into remission or suggest other medications that are less dangerous during pregnancy.
How can treatment help?
There are many types of medications used to treat autoimmune diseases. The type of medicine depends on the type of illness the patient has, its severity, and the symptoms that appear. Treatment can do the following:
Relieve symptoms. For mild symptoms, such as mild pain, some people may use over-the-counter medications such as aspirin and ibuprofen. However, more severe symptoms require prescription medications or even surgery.
Replace vital substances that the body can no longer produce on its own. Some autoimmune diseases, such as diabetes and thyroid disease, can affect the body's ability to produce substances needed to function. In diabetes, insulin injections are necessary to regulate blood sugar levels.
Suppress the immune system. Some medications can suppress the activity of the immune system, and thereby control the disease process and the preservation of organ function.
They are used, for example, to control inflammation in the kidneys in people with lupus.
Thus, treatment includes chemotherapy, given in lower doses than for cancer, and drugs to protect the transplanted organ from rejection (immunosuppressants).
Related book: Immune System Restoration Program
Although symptoms can be mitigated by administering immunosuppressants, their negative effect makes the body easily susceptible to viral infections (influenza, sarcoidosis, etc.), so there are risks of new, even trivial infections that can complicate the patient's condition.
New methods of treating autoimmune processes are constantly being studied.
Source: https://sci-news.ru/2019/autoimmune-disease/
Scleritis
Scleritis is an inflammatory process that affects the entire thickness of the outer connective tissue membrane of the eyeball. Clinically manifested by hyperemia, vascular injection, edema, pain on palpation of the affected area or movements of the eyeball. Diagnosis of scleritis comes down to an external examination, biomicroscopy, ophthalmoscopy, visometry, tonometry, fluorescein angiography, ultrasound (US) in B-mode, computed tomography. Depending on the form of the disease, the treatment regimen includes local or systemic use of glucocorticoids and antibacterial agents. With purulent scleritis, opening the abscess is indicated.
Scleritis is an inflammatory disease of the sclera, characterized by a slowly progressive course. Among all forms, anterior scleritis is the most common (98%). Damage to the posterior parts of the sclera is observed in only 2% of patients.
Options for the course of pathology without necrosis predominate over necrotizing ones, which is associated with a favorable prognosis. In rheumatoid and reactive chlamydial arthritis, diffuse variants of the disease are common.
In 86% of cases of ankylosing spondylitis, nodular scleritis is diagnosed. In 40-50% of patients, pathological changes in the sclera are combined with damage to joints of inflammatory origin, and in 5-10% of cases, arthritis is accompanied by scleritis.
The disease is more common in females (73%). The peak incidence occurs between the ages of 34 and 56 years. In children, the pathology is observed 2 times less often.
Scleritis
The etiology of scleritis is directly related to a history of systemic diseases.
Triggers of scleral damage are rheumatoid arthritis, Wegener's granulomatosis, juvenile idiopathic, reactive chlamydial or psoriatic arthritis, polyarthritis nodosa, ankylosing spondylitis and polychondritis, characterized by a relapsing course.
Less commonly, this pathology develops in the postoperative period after surgical removal of pterygium or traumatic injury. Clinical cases of infectious scleritis in patients with a history of vitreoretinal surgery are described.
Scleritis of infectious etiology is often caused by dissemination of the process from the area of ulceration on the cornea. Inflammation of the paranasal sinuses can also be a source of infection.
The most common causative agents of the disease are Pseudomonas aeruginosa, Varicella-Zoster virus and Staphylococcus aureus. In rare cases, scleritis is of fungal origin. Drug-induced damage to the sclera often develops when taking mitomycin C.
Risk factors are a history of osteoarticular forms of tuberculosis, systemic inflammatory diseases.
From a clinical point of view, ophthalmology distinguishes anterior (non-necrotizing, necrotizing), posterior and purulent scleritis. Non-necrotizing lesions of the sclera can be diffuse or nodular. Necrotizing may or may not be accompanied by an inflammatory process. In some cases, the course of scleritis is characterized by short-term self-terminating episodes.
At the same time, the pathological process in the sclera provokes its necrosis with the involvement of the underlying structures. This disease is characterized by an acute onset; indolent variants are less common. With diffuse scleritis, the entire anterior part of the outer connective tissue membrane of the eyeball is involved in the inflammatory process. Nodular lesions are accompanied by decreased visual acuity.
Anterior scleritis is characterized by a slowly progressive course. This form is accompanied by binocular damage to the organ of vision. Patients note severe pain when touching the area of edema projection, photophobia.
The long course of the disease leads to damage to the sclera along the circumference of the limbus (ring-shaped scleritis) and the occurrence of severe keratitis, iritis or iridocyclitis.
With purulent scleritis, rupture of the abscess membranes is possible, which leads to the development of iritis or hypopyon.
With necrotic damage to the sclera, patients note increasing pain, which later becomes constant, radiating to the temporal region, brow ridge and jaw. The pain syndrome is not relieved by taking analgesics. Necrotizing scleritis is complicated by perforation of the sclera, endophthalmitis or panophthalmitis.
In the posterior form of the pathology, patients complain of pain when moving the eyeball and limited mobility. Postoperative scleritis develops within 6 months after surgery. In this case, an area of local inflammation is formed, which is replaced by necrosis.
A decrease in visual acuity is observed only when the inflammatory process spreads to the adjacent structures of the eyeball or the development of secondary glaucoma.
Diagnosis of scleritis includes external examination, biomicroscopy, ophthalmoscopy, visometry, tonometry, fluorescein angiography, B-mode ultrasound (US), computed tomography.
An external examination of patients with anterior scleritis reveals swelling, hyperemia and vascular injection. The area of edema has defined boundaries. On palpation examination, pain is noted.
Carrying out biomicroscopy for “jellylike” scleritis allows us to identify the area of overhang of the chemosed conjunctiva over the limbus. This area has a red-brown tint and a gelatin-like consistency. Infiltrates with pronounced vascularization can be found on the surface of the cornea.
The method of biomicroscopy with a slit lamp for diffuse scleritis determines the violation of the physiological radial direction of the vascular pattern. In the nodular form, viziometry indicates a decrease in visual acuity.
With purulent scleritis, external examination reveals a purulent infiltrate and vascular injection. Damage to the posterior parts of the sclera is accompanied by swelling of the eyelids, conjunctiva and slight exophthalmos.
The ophthalmoscopy method is used to determine prominence of the optic disc, subretinal lipid exudation, retinal and choroidal detachment caused by the accumulation of exudate.
Ultrasound in B-mode indicates thickening of the posterior part of the outer connective tissue membrane of the eyeball, accumulation of exudate in Tenon's space. Changes in scleral thickness can also be confirmed using CT.
In case of necrotizing scleritis, fluorescein angiography is used to determine the tortuous course, areas of vascular occlusion, and avascular zones.
Carrying out biomicroscopy with a slit lamp allows you to visualize necrotic changes in the sclera and ulceration of the adjacent conjunctiva. The dynamics reveal an expansion of the necrosis zone.
Tonometry in patients with scleritis often reveals an increase in intraocular pressure (more than 20 mm Hg).
The treatment regimen for scleritis includes the local use of glucocorticoid and antibacterial drops for instillation. If the disease is accompanied by increased intraocular pressure, then the therapy complex must be supplemented with topical antihypertensive drugs.
The course of treatment includes taking non-steroidal anti-inflammatory drugs. If they are intolerant, it is recommended to prescribe medications from the group of glucocorticosteroids. For scleritis without necrotic lesions, glucocorticoids and antibacterial drugs must be administered in the form of subconjunctival injections.
An alternative to this method of administration is taking long-acting forms of glucocorticoids.
With the development of scleral necrosis, combination therapy with glucocorticosteroids and immunosuppressants is indicated. In cases of an allergic reaction, antiallergic and desensitizing drugs are used in parallel with these medications.
With the purulent form of scleritis, treatment tactics boil down to massive antibacterial therapy. In this case, oral and subconjunctival routes of administration of drugs from the group of fluoroquinolones, aminoglycosides and semi-synthetic penicillins are used. An additional method of administration is electrophoresis.
If there is no effect of drug therapy, surgical opening of the abscess is indicated. Also, the treatment regimen should include drugs to treat the underlying pathology against which scleritis developed.
If the etiological factor is Mycobacterium tuberculosis, anti-tuberculosis drugs for topical use are considered as auxiliary.
Forecast and prevention of scleritis
Specific prevention of scleritis has not been developed. Nonspecific preventive measures boil down to timely treatment of the underlying pathology, prevention of inflammation of the paranasal sinuses (sinusitis), compliance with the rules of asepsis and antisepsis during surgical interventions.
Patients with a history of systemic diseases need to be examined by an ophthalmologist 2 times a year. The prognosis for life and ability to work depends on the timeliness of diagnosis, the adequacy of treatment, the type of pathogen in the infectious lesion and the form of the disease. The most favorable option is diffuse forms of the disease.
Scleritis caused by Pseudomonas aeruginosa often has a poor prognosis.
Source: https://www.KrasotaiMedicina.ru/diseases/ophthalmology/scleritis
Scleritis: description, symptoms and treatment
Scleritis is an inflammation of the episcleral tissues and scleral tissues on both superficial sides and with deep involvement of the episcleral vessels.
The inflammatory process may involve the cornea, the choroid of the eyeball and adjacent episcleral tissues.
Thus, complications of scleritis can lead to visual impairment, and in extremely advanced stages to complete loss of vision. In half of the patients, scleritis becomes chronic and is seasonal.
Description
Scleritis, or inflammation of the sclera, can manifest as painful redness of the eyes. The most common form of scleritis is inflammation with straightening of the extraocular muscles.
Previously, scleritis was considered a common disease. Clinically, this disease can be divided into four types: diffuse, nodular, necrotic and posterior.
In the diffuse form, scleral edema is present along with dilation of the deep episcleral vessels. The entire anterior part of the sclera is involved in the inflammatory process.
The nodular form of the disease is characterized by the fact that, in addition to swelling of the sclera, numerous or single nodules form on it. One or more nodules may not be visible or palpable in the initial stages.
Necrotizing scleritis is the most severe form of anterior scleritis. It is characterized by severe pain and increased sensitivity of the outer sclera. Basically, necrotizing scleritis is a consequence of systemic severe diseases such as myocardial vasculitis and necrosis.
Posterior scleritis is rare, but its symptoms are quite serious. This form is characterized by retinal detachment and vascular fold. Most often there is loss of vision, as well as pain in the eyes when moving.
Etiology (causes of occurrence):
- Rheumatoid arthritis.
- Injuries.
- Fungus.
- Viruses, bacteria.
- Postoperative complications.
- Lupus.
Risk factors
As a consequence of a systemic autoimmune disease, scleritis is more common in middle-aged or elderly women. This usually occurs in the fourth to sixth decades of life. Men are more likely to develop infectious scleritis than women.
Patients with a history of pterygoid surgery with additional mitomytion or beta-administration irradiation are at higher risk of developing infectious scleritis due to defects in the overlying conjunctival tissue with the formation of calcific necrosis of the sclera.
Bilateral scleritis is more often observed in patients with rheumatic disease. Two or more surgical procedures may contribute to the onset of surgically induced scleritis.
General pathology
Histologically, the appearance of scleritis is expressed by:
- Hyperemic superficial tissue edema.
- Infiltration of tissue.
- Vascular dilations with congested blood, vascular network.
Histologically, there is a chronic and non-granulomatous infiltrate of lymphocytes and plasma cells.
With scleritis, swelling and inflammation are present in all forms of the disease. The inflammation has a granulomatous reaction zone, which can be of two types:
- localized (spot) - can lead to complete loss of vision, near the sclera in this area;
- diffuse (extensive) - the most common course of the disease, inflammation begins in one area and spreads around the circumference until the entire anterior segment is involved in the process.
According to the course of the disease, scleritis can be divided into two types:
- non-granulomatous process (lymphocytes, plasma cells, macrophages)
- granulomatous process (multinucleate giant cells) with or without associated scleral necrosis.
Pathophysiology
Pathophysiological signs are also varied. Scleritis associated with autoimmune disease is characterized by necrosis of the scleral region surrounded by granulomatous inflammation and vasculitis.
There may be a fibrinoid-eosinophilic course with the formation of a granuloma in the center of the inflammatory process.
Also, infectious scleritis is characterized by fibrinoid-exhibition necrosis with deep damage to the walls of blood vessels.
All types of this disease are characterized by an increase in inflammatory T cells, including all types and macrophages. T cells and macrophages infiltrate deep episcleral tissues with B cell clusters in perivascular areas. There may develop a cell-mediated immune response to T cells, both from HLA-DR as well as from IL-2 receptor overexpression.
Differential diagnosis
The onset of scleritis is gradual. This disease has two key symptoms, regardless of the type and form of the disease:
- Pain. There is an increase in pain in the eyeball over several days from mild to very intense.
- Redness of the sclera. May involve the entire eye or a small localized area.
Objective data
Scleritis occurs with the manifestation of a characteristic violet-blue hue of the sclera. Swelling and stretching of the eyeball are also noted.
Examination in natural light differentiates the subtle color differences between scleritis and episcleritis.
Slit lamp biomicroscopy of the sclera shows inflamed vessels.
The visibility of blood vessels and wounded capillaries is also emphasized. Finally, shallow affected vessels can be palpated on the conjunctiva and superficial vessels in advanced stages.
Symptoms
Scleritis, as mentioned above, occurs with a characteristic violet-bluish tint of the sclera. Other features vary depending on the location and extent of scleritis involvement.
There is also severe pain in the eyes, which can be localized in the orbit of the eye. This pain is constant and worsens with eye movement.
During an exacerbation of pain, due to eye movement, the eye muscles tighten and block the rotational movements of the eyeball.
This pain can be significantly worse at night and may cause the patient to wake up during sleep. It also often affects the ears, head, face and jaws.
Diagnostic procedures
- Ultrasound
- Orbital magnetic resonance imaging (MRI). Can be used to detect posterior scleritis.
- Ultrasonographic changes include thickening of the sclera and choroid, scleral nodules, and optic nerve.
Treatment
- Drug therapy
- To treat this disease, NSAIDs are prescribed - non-steroidal anti-inflammatory drugs, which are the first-line agents for mild to moderate scleritis.
- Non-selective cyclooxygenase inhibitors or selective inhibitors such as flurbiprofen, indomethacin and ibuprofen may be used as adjunctive therapy.
Indomethacin can be prescribed at a dosage of 50 mg, three times a day.
Ibuprofen at a dosage of 600 mg, three times a day.
The use of oral NSAIDs is not advisable, and patients are warned about gastrointestinal (GI) side effects (stomach bleeding).
Patients with impaired renal function should be warned about the toxicity of the drug.
Corticosteroids may be prescribed to relieve ocular inflammation if the patient does not respond to COX inhibitors. A typical starting dose may be 1 mg/kg/day of prednisone. Intravenous bolus injection of methylprednisolone in 0.
5-1 mg may initially be needed for severe scleritis.
Side effects of steroids include: decreased resistance to infection, stomach irritation, increased eye pressure, osteoporosis, weight gain, hyperglycemia and mood changes.
In addition to the main treatment, consultation with a rheumatologist is strongly recommended. Patients with rheumatoid arthritis are additionally prescribed methotrexate.
Patients with Wegener's granulomatosis may require cyclophosphamide or mofetil.
Cyclosporine is nephrotoxic and, thus, can be used as an adjuvant therapy to relieve the inflammatory process with fewer side effects.
Nevertheless, the risk of hematological complications is quite high, therefore, in parallel with the treatment of the underlying disease, it is necessary to take hepatoprotective drugs (Esensiale, Gepobene, etc.).
Also, all patients on therapy should take immunomodulatory drugs and closely monitor the development of systemic complications.
Surgery
Clinical examination is usually sufficient to make a diagnosis. A formal biopsy may be performed to rule out a neoplastic or infectious cause. Small corneal perforations can be repaired with contact lenses or surgical glue.
Primary indications for surgery include scleral perforation or the presence of excessive thinning of the sclera with a high risk of rupture.
Complications
- Peripheral keratitis.
- Cataract.
- Glaucoma.
- Central stromal keratitis.
- Opaque fibrosis.
- Scleritis with herpes zoster.
Features of scleritis in children
In children, this disease develops quite rarely. And often parents confuse it with conjunctivitis and other inflammatory diseases of the eye, thereby aggravating the course of the disease. Therefore, at the first signs, such as swelling, a characteristic hue and pain, you must immediately contact an ophthalmologist for an accurate diagnosis and immediate treatment.
Source: http://r-optics.ru/information/sklerit_opisanie_simptomy_lechenie-276