- In addition, other complications that the disease contributes to cause many problems and damage health.
- One of the most common diseases is cryptorchidism .
- Cryptorchidism is a condition in which one or two testicles are not descended into the scrotum and are located in the abdominal cavity or in the inguinal canal.
- Sometimes the testicle can be located in the groin, in a subcutaneous place in the thigh, or perineum.
- Localization of cryptorchidism can be right-sided (more common than others), left-sided or bilateral.
Disease history
The formation of the vital functions of the body of any person at the embryonic stage occurs in the first trimester of pregnancy. Lack of vitamins and endocrine disorders of the mother's body can lead to the development of disease in the fetus due to impaired development of the gonads.
In the eighth month of pregnancy, during normal development of the fetal genital area, the testicles descend through the inguinal canal from the abdominal cavity into the scrotum. If this does not happen, then the child is born with the pathology cryptorchidism.
For various reasons, the testicle is delayed on its way to its physiological location - the scrotum.
Cryptorchidism can be congenital or acquired.
Prevalence and significance
The disease cryptorchidism in newborn boys is quite common: in 5% of babies. By three months from birth, about 2% of patients remain with undescended testicles. There is definitely a more frequent development of cryptorchidism in premature infants.
Among genitourinary diseases in children from birth, cryptorchidism is the most common pathology.
Cryptorchidism must be treated. The disease can cause infertility and also contribute to the formation of a malignant testicular tumor.
Risk factors
The main risk factors for the disease are:
- presence of diseases in men in the generation;
- taking hormonal drugs (estrogens) by the mother during pregnancy;
- early birth (prematurity) of a child.
In addition, cryptorchidism is more common at the birth of the first premature baby than in subsequent children.
Causes and consequences
The exact causes of the disease are unknown.
But boys who are diagnosed with:
- narrowness (obstruction) of the inguinal canal;
- short spermatic cord;
- intra-abdominal adhesions;
- underdevelopment of the associated testicular system.
Often, the development of the disease is paralleled with the presence of genetic diseases: Down syndrome, mutation of the GTD gene, pathology of the development of the abdominal anterior wall. Premature boys up to 900 g in weight are all born with cryptorchidism, since the descent of the testicles into the scrotum occurs at later stages of development.
Symptoms and diagnostic methods
The main symptoms of the disease are:
- absence of testicles in the scrotum;
- asymmetry, flattening of the scrotum upon visual examination;
- aching pain in the groin area, in the abdomen;
- pain in the abdominal cavity with straining, constipation, tension in muscle tissue.
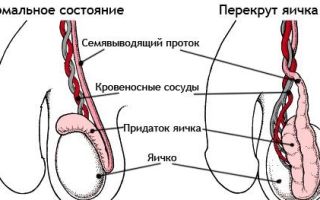
In addition, with cryptorchidism, torsion of the spermatic cord is most often observed.
In combination with a hernia in the groin, the testicle may be pinched, which leads to severe pain.
Important! If you experience acute pain in the groin area, you should consult a doctor as soon as possible. If a testicle is pinched, its death is inevitable within a few hours.
This phenomenon is caused by the hernia squeezing the bloodstream leading to the testicle.
Diagnostics
A doctor can diagnose cryptorchidism by palpating the scrotum. After the fact of the absence of a testicle in the scrotum is established, the places of its possible location are probed. If they are not found, then using ultrasound, MRI or other computer studies, they find the testicle inside the peritoneum or groin area.
- With the help of laparoscopy, examinations can be more effectively carried out to confirm or exclude the presence of a testicle.
- Video: “What is cryptorchidism?”
Treatment
By the age of one year, the undescended testicle must be lowered into the scrotum through surgery. This is due to the fact that the testicle will not descend on its own, and, being in a warm environment in the abdominal or inguinal cavity, it can atrophy and lose its functions.
Treatment with drugs
Hormonal drugs are prescribed at an early age of the child. However, such therapy has a low percentage of effectiveness. When medications are discontinued, a relapse of the disease often occurs. The most effective method of treating cryptorchidism is operable prolapse.
Surgery
Surgery to treat cryptorchidism is called orchiopexy.
Operation sequence:
- the surgeon makes an incision in the groin;
- finds the testicle and lowers it into the scrotum;
- fixes the location of the testicle by sewing it to the bottom of the scrotum.
After orchiopexy, in rare cases, complications are observed: damage to the blood vessels supplying the testicle occurs, which can lead to atrophy or resorption of testicular tissue.
If cryptorchidism is treated in an adult male, the undescended testicle is removed, since it is not able to perform the function of sperm formation. However, such a pathology may not always be the cause of infertility: often the second testicle has good sperm production and performs the reproductive function quite successfully.
Important! One of the main indicators of the effectiveness of surgery for cryptorchidism is its timely implementation.
- If the testicle descends in a timely manner, the probability of its productivity remains in 90 cases out of a hundred.
- Video: “Surgical treatment of abdominal cryptorchidism”
Treatment with folk remedies
It is useless to treat cryptorchidism with traditional medicine. It is not recommended to resort to this method, since in this case it can only cause harm.
Diet
It is not advisable to recommend any diet to patients who are infants, since babies at this age are breastfed and the introduction of lean foods into the diet.
If cryptorchidism is present in men, then the cause of the deviation is often a lack of the hormone testosterone. It is necessary to include in the diet such foods as nuts, seafood, vegetables, fruits, berries, pearl barley porridge, dried fruits.
It is believed that even a balanced diet will not lead to the descent of the testicle to its natural place, but can help maintain functionality.
Prevention
It is possible to prevent the occurrence of complications in the presence of cryptorchidism. Such measures include timely surgical intervention.
Prevention of the occurrence of the disease itself can be carried out by the mother during pregnancy:
- eliminate bad habits;
- Healthy food;
- avoid diseases (flu, rubella) during pregnancy;
- use medications as little as possible;
- regular fresh air.
If there is a genetic predisposition to the disease, preventive measures will not help, but this is not an indicator to avoid the diet and daily routine for a pregnant woman.
Forecast
In the presence of cryptorchidism, surgical intervention has a favorable prognosis. In most cases, the reproductive function of a descended testicle is preserved. However, the operation should not be delayed.
If you refuse surgery, serious consequences of the disease may occur:
In addition, in the presence of bilateral cryptorchidism, a man’s ability to bear children is reduced.
Thus, cryptorchidism is a fairly common congenital disease. It is acquired when the cord is pulled and raised to the upper part of the groin area, and such cryptorchidism is false.
Despite the fact that testicular descent is mainly performed surgically, the prognosis for treatment in most cases is favorable. Spontaneous prolapse at an early age occurs infrequently if the baby is born full term.
Conclusion
It is so inherent in nature that the male genital organs have two testicles, and if one or none is observed, this phenomenon is a deviation and should be treated. If a boy has one normally functioning testicle, then for normal hormonal development in adolescence, treatment and consultation with an endocrinologist should be carried out.
Source: https://kakbyk.com/bolezni/narushenie-polovogo-razvitiya/lechenie-kriptorkhizma-u-muzhchin.html
Causes and treatments for cryptorchidism in boys and adult men
Unfortunately, not in all cases the development of the male gonads occurs normally. One of the most common anomalies is the pathology of testicular descent - cryptorchidism.
According to various authors, the prevalence of the disease in the population reaches 5%, and it is more often detected in premature boys.
Timely treatment often allows almost complete restoration of dysfunction, so when the first symptoms appear, you cannot delay going to the doctor.
Definition and classification
Cryptorchidism is a pathology of the process of the testicle descending to its correct position (into the scrotum) during intrauterine development. Interest in this disease is associated with a high risk of complications characteristic of older age, among which infertility, cancer and erectile dysfunction (impotence as an extreme manifestation) are of particular importance.
Depending on the level and type of disorder, the proposed treatment options may vary. There are 2 following forms of developmental delay:
- Retention - the testicle remains within the abdominal cavity or inguinal canal.
- Ectopia - it deviates from the correct trajectory and can even be located under the skin of the pubis, thigh and perineum.
In practice, clinical classification is used. It implies the following division:
- True cryptorchidism in men:
- ectopia – femoral, inguinal or perineal;
- abdominal retention (retroperitoneal);
- inguinal retention – testicle in the inguinal canal;
- unilateral or bilateral cryptorchidism;
- combined.
- False cryptorchidism is a condition in which the testicle can be returned to the scrotum, but it reflexively occupies a more elevated position (due to muscle hypertonicity).
Some boys experience spontaneous prolapse in the first months of life (full recovery), but they are still subject to dispensary registration for the indicated period. Acquired cryptorchidism is much less common.
Reasons for development
After the 6-7th week of intrauterine development, the fetus begins to develop sexual characteristics under the influence of genetic (SRY triggers the differentiation of gonads into male) and neurohumoral factors (testosterone and its metabolites, as well as maternal factors). The final position of the testicles will depend on a multi-step process of interaction between various structures. Its violation at any stage can cause non-descending.
Thus, the etiology of the disease is not always clear. Cryptorchidism often develops in boys for the following reasons:
- Chromosomal (genetic) disorders: GTD gene mutation, Down syndrome, Klinefelter syndrome, Noonan syndrome, X trisomy.
- Violation of pregnancy (prematurity) or taking pharmaceuticals (non-steroidal anti-inflammatory drugs - Ibuprofen, Paracetamol, Aspirin).
- Insufficient synthesis of luteinizing hormone, testosterone (and its metabolites), as well as excess estrogen in the fetus.
- Maternal diseases during pregnancy: influenza, rubella, toxoplasmosis, diabetes mellitus, thyroid dysfunction.
- The presence of a mechanical barrier in the form of fibrous cords, adhesions, anomalies in the development of the neurovascular bundle (the internal spermatic artery is especially significant), an anatomically narrow inguinal canal or no guide ligament at all.
- Testicular dysgenesis syndrome (impaired formation of testicular tissue due to genetic and external causes).
Attention! We must also not forget that smoking and hereditary diseases of the father directly affect spermatogenesis. The chances of healthy offspring are many times higher for parents without bad habits and risk factors (comorbidities, standard of living, environment), so medical genetic counseling remains more relevant than ever.
Possible symptoms
The main symptom of the disease is the absence of a testicle in the right place, that is, the scrotum. In most cases, this is detected in the first weeks of a child’s life, so cryptorchidism in adults is a rare phenomenon.
At this stage, differential diagnosis between true, false variants and ectopia is necessary. In this case, by palpation (that is, by touch), the localization of the testicle, its size and consistency are revealed, which is compared with the data of the parents’ medical history.
With false cryptorchidism, the gonads may periodically descend into the scrotum. To check it, you need to suppress the cremasteric reflex (develops when touching the skin of the inner thigh) as follows:
- Examination with the patient supine and legs crossed.
- The doctor places his hand directly above the pubic symphysis.
- Then he touches the skin of the inner thigh or moves his hand to the scrotum.
You can try to “move” the groin area somewhat towards the scrotum, as if pushing the gonads there. Unilateral absence of a testicle (for example, right-sided cryptorchidism) often indicates its agenesis, ectopia, or even atrophy. To make a diagnosis, consultation with an experienced urologist is required.
Cryptorchidism in adolescents with undescended testicles (bilateral) can be suspected by indirect signs. Among them, the most significant are the following:
- wide (female) pelvis;
- gynecomastia (growth of mammary glands in men);
- high timbre of voice;
- congenital anomalies: cleft palate or lip, heart defects, anal atresia, umbilical hernia;
- concomitant phimosis, hypospadias;
- disturbances in the appearance of sexual characteristics during puberty.
If the testicle was not found in the scrotum, you need to carefully palpate the iliac and pubic areas, the inner surface of the thighs, the base of the penis and the perineum as a whole. Any protrusion or mobile (usually painless) formation is a possibility of ectopia.
Diagnostics
Despite the fact that the main method for distinguishing an undescended testicle is palpation (feeling), independent diagnosis is impossible. A medical examination should be carried out in the first days or weeks of the boy’s life. It includes the following activities:
- The main ones: palpation, ultrasound of the scrotum and inguinal canal (less often - CT), contrast vasography (to rule out the complete absence of the testicle - anorsism).
- Additional (as indicated by the doctor, usually before surgery):
- general blood and urine analysis;
- biochemical blood test;
- HIV tests, determination of blood group and Rh factor;
- Ultrasound of the abdominal organs;
- karyotyping or sex chromatin study - the genetic sex of the child;
- hormonal profile.
The intra-abdominal or inguinal location of the testicles cannot be determined without diagnostic laparoscopy (performed under general anesthesia). However, there must be compelling reasons for such intervention.
Treatment methods
If there is a clearly established diagnosis, treatment is not difficult. Usually, newborn boys with this pathology are observed for a maximum of 1 year - further waiting can be fraught with histological damage to testicular tissue (risk of infertility).
Medication
Drug therapy is not the preferred method of treatment. It is based on the use of hormonal drugs containing human chorionic gonadotropin (hCG) or gonadoliberin (GnRH).
It is believed that the higher the testicular retention occurred, the less effective the use of medications. In addition, clinical studies have not confirmed the safety of this method due to frequent apoptosis of stem (germ) cells.
Before surgery, it may be necessary to create favorable conditions for the formation of a cosmetic defect that is invisible in the postoperative period. For this purpose, antibiotics are used (according to indications), anesthetics and anesthetics (Ketamine, Atropine, Sevoflurane, Lidocaine), and infusion solutions.
Operational
The technique will differ depending on the type of cryptorchidism. But in any case, the only way to return the testicle to its place is to undergo surgery. The following intervention options are possible:
TesticlesOperationHighlights| Palpable | Orchifuniculolysis + orchipexy; according to Petrivalsky-Schemaker | The success rate of the operation is more than 92% thanks to optical magnification and microsurgical instruments. The doctor performs an inguinal approach, cutting through the tissue up to the anterior wall of the canal. The tissues are mobilized, a bed is formed between the skin of the scrotum and the muscular layer, where the testicle is lowered. |
| Non-palpable | Orchidolysis + orchipexy. Fowler-Stevens procedure in patients under 10 years of age with bilateral undescended disease. | If the testicles cannot be detected during physical examination, a revision (surgical examination) of not only the groin, but also the abdominal area may be required. The probability of successful preservation of the testicles, depending on the choice of intervention, ranges from 40 to 90%. |
If intra-abdominal cryptorchidism has been confirmed, laparoscopic techniques are used to bring the gonads into the scrotum. After this, the child is left with 3-4 small round scars, which will significantly decrease in size with age. If the testicle atrophies, it must be removed - an operation called orchiectomy.
Complications
Although cryptorchidism is rarely accompanied by pain and may not cause discomfort, the problem cannot be ignored. The following complications may develop:
- inflammation of the undescended testicle and surrounding tissues;
- torsion;
- pinching (severe pain);
- malignancy – malignancy;
- decreased fertility (the risk of infertility is especially high with a bilateral process);
- impaired potency and libido.
Currently, this disease is considered a non-disease diagnosis. But keep in mind that only those young men who have been confirmed to have an abdominal location of an undescended testicle are not accepted into the army.
Source: https://UroMir.ru/andrologija/zabolevanija-testikuly/kriptorhizm.html
Cryptorchidism
Cryptorchidism is a congenital anomaly in which at the time of birth a boy lacks one or both testicles in the scrotum, which is due to a delay in their descent along the inguinal canal from the retroperitoneum. The pathology is manifested by asymmetry of the scrotum, the absence of a testicle during palpation, and aching pain in the groin or abdomen. Diagnosis includes ultrasound of the scrotum, MRI, testicular scintigraphy, angiography of the abdominal aorta and venography of the testicular vein. The main method of treating cryptorchidism is surgical; the testicle is brought down and fixed to the scrotum.
In modern andrology, undescended testicles or cryptorchidism is the most common congenital anomaly, occurring in 4% of full-term and 10-20% of premature newborn boys.
During the first 6 months of life, 75% of children born with cryptorchidism experience spontaneous testicular descent, probably due to a gradual increase in testosterone levels. By the end of the 1st year of life, the pathology persists in only 1% of boys.
In the future, in the absence of medical assistance, the likelihood of spontaneous descent of the testicles into the scrotum is unlikely. Delayed surgical treatment increases the likelihood of developing male infertility and testicular cancer in the future.
Cryptorchidism
The reasons for delayed testicular descent and the development of pathology are not precisely known. Endocrine, mechanical and genetic factors are considered as possible prerequisites.
Endocrine mechanisms for the development of the disease include the presence of hormonal imbalance in a pregnant woman (in particular, diabetes mellitus type 1, 2 or gestational, dysfunction of the pituitary gland, thyroid gland) or testicles in the embryo.
These conditions can inhibit the timely descent of the testicles into the scrotum and cause the development of bilateral cryptorchidism.
Mechanical factors include narrowness or obstruction of the inguinal canal, shortening of the testicular vessels or spermatic cord, underdevelopment of the testicular ligaments, intraperitoneal adhesions, etc.
In some cases, cryptorchidism is associated with a mutation of the GTD gene (306190, Xp21), Down syndrome, and intrauterine developmental defects of the anterior abdominal wall. Preterm birth and prematurity significantly increase the likelihood of the disease.
Cryptorchidism is detected in all premature boys weighing less than 910 g and in 17% with a body weight of more than 2040 g.
In some cases, cryptorchidism is acquired. Thus, a wide inguinal ring or trauma to the scrotum can cause migration of an initially normally located testicle into the groin area or abdominal cavity.
The laying and formation of testicles (testicles) in the fetus occurs in the abdominal cavity. In the last trimester of pregnancy, the testicles descend into the scrotum along the inguinal canal.
It is believed that timely spontaneous retraction of the testicles is determined by a number of mechanisms - intra-abdominal pressure, local testosterone levels, the state of the testicular ligament and its attachment to the scrotum.
After the birth of a boy, further normal development of the testicles is possible only if they are in the scrotum, where the temperature is 2-3°C lower than in the abdominal cavity. This temperature difference is a necessary condition for normal spermatogenesis. Typically, an undescended testicle is smaller in size than a timely descended testicle.
There are false and true cryptorchidism. With a false type of pathology (migrating testicle), under the influence of muscle tension or cold, the testicle can move into the inguinal canal or abdominal cavity. False cryptorchidism occurs in 25-50% of all cases.
It is characterized by symmetry and normal development of the scrotum; migration of the testicle to the area of the inguinal ring or the lower third of the inguinal canal; the possibility of unhindered descent of the testicle into the scrotum during palpation or its spontaneous descent under the influence of heat or in a relaxed, calm state of the child.
Testicular migration is a variant of the physiological norm and is explained by the small diameter of the testicle compared to the diameter of the external inguinal ring. Therefore, when the corresponding muscles contract, the testicle is easily pulled up to the inguinal fold. False cryptorchidism does not require treatment and disappears on its own at puberty.
True cryptorchidism is said to occur when it is impossible to manually lower the testicle into the scrotum. In this case, the testicle is most often located in the inguinal ring (40%), in the inguinal canal (20%), and abdominal cavity (10%).
If one of the testicles is undescended, a diagnosis of unilateral testicles is made; if the descent of both is delayed, a diagnosis of bilateral true cryptorchidism is made.
Bilateral anomaly is often combined with hypogonadism, hypothalamic-pituitary insufficiency (hypopituitarism), and inguinal hernia.
A condition such as testicular ectopia should be distinguished from true cryptorchidism. In the case of ectopia, the testicle, having passed the inguinal canal, does not enter the scrotum, but the perineum, the medial surface of the thigh, the anterior abdominal wall, and rarely, the dorsal surface of the penis. With testicular ectopia, even after treatment, most patients are infertile.
The main manifestation of the pathology is the absence of one or two testicles in the scrotum, which the andrologist determines by palpation. In this case, the scrotum looks underdeveloped, flattened or asymmetrical.
With cryptorchidism, there may be aching and nagging pain in the groin or abdomen.
When the testicle is localized in the abdominal cavity, pain, as a rule, appears only in puberty and can intensify with muscle tension, straining, constipation, and sexual arousal.
Cryptorchidism increases the risk of developing testicular cancer (seminoma), impaired fertility (decrease in the number of sperm according to the spermogram, low quality of sperm and its fertilizing ability).
With bilateral pathology, about 70% of men are infertile.
In addition, cryptorchidism can cause the development of testicular torsion, more precisely the spermatic cord, formed by blood vessels, nerves and the vas deferens.
In the case of a combination of the disease with an inguinal hernia, strangulation of the testicle along with intestinal loops in the inguinal ring cannot be ruled out.
These conditions are accompanied by sharp pain due to impaired blood supply to the testicle and its death within the next few hours.
When an undescended testicle is located in the groin, the pubic bone may press on it, which, in turn, increases the risk of injury to the gonad.
Cryptorchidism is detected by examination and palpation of the scrotum. In the absence of a testicle, the scrotum on the corresponding side looks underdeveloped and flattened. With abdominal retention, the testicle cannot be palpated; in other cases, the testicle is found in the inguinal canal.
With the inguinal location of the testicle, it is to a certain extent mobile and displaceable; with false cryptorchidism, it is easily displaced into the scrotum. In the case of true cryptorchidism, it is not possible to reduce it to the scrotum.
The absence of a testicle is confirmed by an ultrasound scan of the scrotum.
If it is impossible to palpate to determine the location of the testicle, they resort to performing an ultrasound of the abdominal cavity and groin area, and plain radiography of the abdominal cavity.
If ultrasound is uninformative, contrast-enhanced MRI or CT may be required, and in difficult cases, diagnostic laparoscopy to confirm abdominal testicular retention or establish monorchism or anorchism.
If it is impossible to palpate and instrumentally identify both testicles, it is necessary to exclude male pseudohermaphroditism, for which genetic tests, testing of testosterone, and gonadotropic hormones are carried out.
If the pathology is false, no treatment is required. Correction of true cryptorchidism is carried out by pediatric endocrinologists and urological surgeons.
Treatment for cryptorchidism begins when the child reaches 9 months of age, before this period, counting on the possibility of spontaneous descent of the testicle into the scrotum.
Drug therapy is carried out using intramuscular injection of human hCG or intranasal administration of gonadorelin.
As a result of conservative therapy, it is possible to achieve testicular descent in 30-60% of patients.
Hormonal drug treatment is contraindicated during puberty, when there is an increase in the level of testosterone and gonadotropic hormones.
If conservative therapy fails, surgical intervention is indicated by the age of 15-24 months - orchiopexy (surgical reduction of the testicle into the scrotum).
During the operation, a testicular biopsy is required to exclude malignant processes and gonadal dyskinesia. Intervention is absolutely necessary in case of testicular torsion, strangulation, inguinal hernia, or ectopic testicle.
If hypotrophy or necrosis of the gland is detected, resection of the testicle or its removal is performed - orchiectomy.
In the latter case, as well as with anorchism at an older age, a donor testicle transplant or implantation of an artificial testicle is required for cosmetic correction of the defect.
In the case of early (up to 2 years) testicular descent or unilateral cryptorchidism, the risk of subsequent complications is significantly reduced. Infertility subsequently develops in 20% of patients with unilateral cryptorchidism and in 70-80% of patients with bilateral cryptorchidism.
In the absence of at least a single, normally functioning testicle, boys require treatment by an endocrinologist for normal sexual and physical maturation according to the male type.
In the future, parents, and then the teenager, are recommended to conduct a self-examination of the testicles to detect possible tumor processes. Primary prevention has not been developed.
Source: https://www.KrasotaiMedicina.ru/diseases/zabolevanija_urology/cryptorchidism
Cryptorchidism - causes, signs, symptoms, treatment
Cryptorchidism in children or adults is a disorder in which one or both testicles do not descend into the scrotum for a certain period. It is normal for the testicles to droop during the period from fetal development in the womb to one year after birth. The disease is dangerous due to complications that can affect the reproductive function of an adult.
Online consultation on the disease “Cryptorchidism”.
Ask a question to the specialists for free: Urologist.
As is known, the formation and formation of testicles in a boy occurs in the abdominal region. They should pass through the canal in the groin and descend into the scrotum in the last months of the mother's pregnancy. Experts believe that testicular drooping occurs due to several reasons:
- a certain pressure in the abdominal cavity;
- testosterone levels;
- attachment of the organ to the scrotum.
The descent of the testicles into the scrotum is necessary for their further development and ensuring spermatogenesis, as well as the normal functioning of the genital organs, because in the scrotum the temperature is 2-3 degrees lower than in the body. Accordingly, an organ that is not descended in time may be smaller in size than a normally developed one.
Causes of development in children
The causes of cryptorchidism in a child may be as follows:
- hormonal. They appear in the mother’s womb, which can be caused by problems in the endocrine system in the fetus or mother. Diabetes mellitus can also cause the disease. Pathologies of the endocrine gland are especially dangerous in the last trimester of pregnancy;
- genetic predisposition. Cryptorchidism can develop if male relatives have been diagnosed with this disease;
- disturbances in anatomy. Cryptorchidism in children can be caused by mechanical damage to the testicles during their passage through the narrow inguinal passage. Also, anomalies can be caused by circulatory disorders (due to deformation of nearby vessels);
- early birth. Cryptorchidism in children most often develops when they are premature (especially if the child weighs less than 1 kg) or during multiple births;
- mutations. Most often, the disease affects patients with Down syndrome, which, in turn, causes pathologies in the development of the abdominal walls.
Causes of illness in adults
Cryptorchidism in men, which has code Q53 according to ICD-10, usually develops due to mechanical obstacles that prevent the organ from descending into the scrotum. Visually, you can even identify the problem yourself. The causes of unilateral or bilateral disease in adults are divided into 3 types:
- pathologies in the development of the vascular pedicle;
- pathologies of the endocrine system;
- peritoneal fusion.
Right-sided cryptorchidism, like left-sided cryptorchidism, is rare in adults. It can be detected during an examination by a urologist or based on ultrasound results.
Cryptorchidism
Symptoms
The symptoms of cryptorchidism are:
- absence of one or both testicles in the scrotum;
- visual underdevelopment, asymmetry of the scrotum;
- aching and pulling pain in the abdomen or groin, which intensifies with excitement and straining.
Symptoms of cryptorchidism may be exacerbated by torsion of the spermatic cord. If an undescended testicle is complicated by the presence of a hernia, it will be strangulated and, if left untreated, may die. The location of the testicles in the groin is also dangerous, because there they can be injured due to the presence of the pubic bone nearby.
Kinds
Bilateral and unilateral cryptorchidism can be of the following types:
- false. Involves placing the testicle in a reservoir in the groin. Since this reservoir is located in the abdominal cavity, the patient feels it during abdominal tension. False cryptorchidism assumes normal functioning of the scrotum, and a slightly reduced defective organ, in the absence of hypothermia, has a high chance of descending on its own. Typically, a disease such as false cryptorchidism does not require treatment;
- true. This form of the disease means that the testicle is located in the inguinal canal. Doctors distinguish between unilateral and bilateral cryptorchidism. The latter subtype can often be accompanied by other diseases of the reproductive system. Visually, the pathology is detected due to the asymmetry of the scrotum, and the undescended organ can be found by palpation;
- acquired. It is triggered by injuries to the groin area, which cause movement of the testicles, as well as long wearing of a bandage after surgery to remove a hernia. Requires treatment and can be diagnosed at any age;
- ectopia. Provides for the location of the testicles in any place except the scrotum. Accordingly, pubic, femoral, and perineal cryptorchidism are distinguished.
Testicular torsion
Left-sided cryptorchidism is more common due to the structural features of the male reproductive system.
Consequences
The most common side effect after the discovery of congenital or acquired cryptorchidism (in the absence of treatment) is male infertility - it is diagnosed in 70% of patients. Also leading among the consequences are:
- bilateral form of the disease. Develops as a result of mechanical damage or circulatory pathologies. It can also be caused by overheating of the groin area or physical inactivity. In this case, the spermogram shows a low number of sperm. To avoid such a complication, young children need to undergo surgery before the age of 1.5 years;
- testicular cancer. Someone who suffers from cryptorchidism is half as likely to get it. Often, tumor damage to a healthy testicle is observed;
- disruptions in hormonal levels. This can cause a slowdown in the appearance of secondary sexual characteristics, obesity, and the development of an effeminate physique. Body hair may stop growing;
- torsion It is a pathology of blood circulation in the testicles, which is accompanied by pain in the groin area, high fever or even vomiting. Visually determined by blue discoloration of the scrotum.
Diagnostics
Diagnosis of pathology includes:
- examination by a doctor. He interviews the patient and palpates the scrotum and groin to determine the position of the testicle;
- examination using ultrasound. Used to obtain a more complete picture of the pathology;
- hormone tests. Play a supporting role in helping to determine whether a patient needs hormone therapy;
- laparoscopy. Can be used for the abdominal form of the disease. It involves introducing air into the abdominal area through a trocar, and then through a camera lens, the image from which is visible on the monitor.
Treatment
Treatment of pathology should begin as quickly as possible to avoid complications. Treatment may be:
- conservative. It involves taking vitamins and hormones, which helps move the testicles to the scrotal area. Usually used to treat pathology in children under one year of age;
- operational. It involves surgery, which can take place under local or general anesthesia. Doctors will cut the groin area to lower the testicle and secure it in the scrotum.
If conservative treatment was unsuccessful, then the child at the age of 1–2 years is prescribed orchiopexy. Before surgery, a testicular biopsy is required to detect malignant tumors and other abnormalities. Patients with torsion of the seminiferous tubules, ectopia or hernia in the groin require surgery.
Surgery for cryptorchidism can be of two types:
- open. During the operation, an incision is made in the patient's abdomen, doctors find the undescended testicle and lower it in one or more stages;
- laparoscopic. Several punctures are made in the patient's abdomen near the testicle to direct it to the scrotum area. Often, when performing an operation on teenagers or older men, the testicle needs to be removed, because it has not been viable for a long time, and a tumor may appear in it. Laparoscopic surgery can also help remove a hernia in the groin.
If a necrotic process of the gland is detected, then doctors will remove the testicle. If the operation is carried out after the patient grows up, then after it it is necessary to eliminate the defect by transplanting a donor testicle or inserting an artificial organ.
Treatment of the disease in a hospital setting lasts up to a week, after which the patient is discharged home. Even after surgery, patients should be periodically examined by a doctor, as they have an increased risk of developing cancer. Also, as a preventive measure, they are recommended to conduct self-examination of the testicles.
If the disease was detected and cured in patients under 2 years of age, then they have a fairly low risk of negative consequences - for example, up to 20% of those who had an undescended testicle can develop infertility. If at least one testicle does not function normally, then the boy should be registered with an endocrinologist.
Source: https://SimptoMer.ru/bolezni/muzhskie-zabolevaniya/1582-kriptorkhizm-simptomy
Cryptorchidism
Cryptorchidism is the failure of one or two testicles to descend into the scrotum. Cryptorchidism in men can have serious consequences associated with the risk of infertility and the development of cancer.
The content of the article:
When the fetus develops within normal limits, in the eighth month of pregnancy inside the mother’s womb, the boy’s testicles descend from the abdominal cavity into the scrotum. Therefore, cryptorchidism is observed in 30% of premature male children.
A testicle that has not descended may remain directly in the abdominal cavity, and there are also cases of it stopping at various places on the way to the scrotum.
There are deviations when the testicle moves, and it ends up in the perineum, on the surface of the thigh, in the superficial pocket of the inguinal canal; its location in this case can only be detected using ultrasound. This pathology is called ectopic testicle.
It is noteworthy that cryptorchidism disappears in 80% of cases in the first 12 months of life: the testicle descends on its own, without the use of medications or surgery. Therefore, operations are not performed before the age of 1 year.
Classification of cryptorchidism
Cryptorchidism is classified according to various criteria. First of all, starting from the place where the undescended testicle is located, the following types of cryptorchidism are distinguished:
- intra-abdominal: the testicle remains where it was formed - directly in the abdominal cavity;
- inguinal (inguinal) - located between the outer and inner inguinal ring in the inguinal canal;
- ectopia: the testicle deviates significantly from its path; it can be found in the perineum, on the thigh, at the base of the penis, in the groin, on the pubis or in another part of the scrotum;
- anorchism: testicles are completely absent;
- false cryptorchidism (in principle, does not apply to the manifestations of cryptorchidism): the testicle is not allowed to fully descend by the muscles that raise it; the testicle is palpable; Unlike true cryptorchidism, it can be guided by hand into the correct position, but after a while it takes its original position. The testicle can sometimes descend on its own, especially if the child is in a relaxed state. Testicular migration may be caused by the large size of the inguinal ring compared to the size of the testicle. This anomaly does not require intervention and goes away on its own.
There is also a distinction between congenital and secondary cryptorchidism. The latter occurs after birth when the testicle/both testicles rise from the scrotum and do not descend back. Sometimes secondary cryptorchidism is acquired after trauma to the scrotum.
There are right-sided, left-sided and bilateral cryptorchidism. Testicles are palpable and non-palpable, depending on whether they can be palpated during examination or not.
Causes of cryptorchidism
There are several factors that can cause the appearance of cryptorchidism. First of all, these include premature birth.
In premature male infants and newborns weighing less than 2400 g, undescended testicles are many times more common than in infants weighing more than 2.5 kg at birth.
There is also a genetic predisposition to this pathology. The risk of multiple pregnancies also increases.
A very important factor is the imbalance of hormones in the body of a pregnant woman, which provokes improper production of hormones in the fetus. There are several reasons that disrupt a woman’s hormonal levels:
- diabetes mellitus, abnormal functioning of the thyroid gland;
- taking painkillers and antipyretics (especially in the first trimester);
- taking certain medications that affect hormone balance (steroids, oral contraceptives);
- eating certain foods that contain phytoestrogens (beer, soy products);
- working with hazardous substances (manufacturing, hairdressing salons, etc.).
There are also mechanical factors. Features of the inguinal canal (very narrow, impassable), adhesions in the abdominal cavity, insufficiently long spermatic cord or testicular vessels, poorly developed testicular ligaments, and insufficient blood supply to the testicles are often identified.
Cryptorchidism occurs in conjunction with other symptoms of intrauterine growth retardation or disturbance. Most often, undescended testicles can be accompanied by Down syndrome, pathologies of the shape of the skull and chest, curvature of the spine, widening of the bridge of the nose, malocclusion, etc.
Symptoms of cryptorchidism
The main symptom of cryptorchidism becomes obvious upon visual examination. The scrotum does not look symmetrical and developed; it is flat on one or both sides. During palpation, one or two testicles are not detected.
Also, a symptom of cryptorchidism in men can be aching pain localized in the abdominal cavity or groin, depending on where the testicles are located.
If in early childhood (up to 18 months) the problem was not corrected, in the puberty period, when the testicle is localized in the abdominal cavity, abdominal pain occurs, as well as with excitement, heavy physical exertion, and during defecation when straining.
Cryptorchidism has very serious complications. This is due to the fact that the necessary temperature regime for the testicles is created in the scrotum. If the testicles remain in the abdominal cavity for 18 months, where the temperature is 2-3 degrees higher than the scrotum, then they do not undergo any changes.
But if this period increases, irreversible changes occur, sperm production stops, which, with unilateral cryptorchidism, significantly reduces fertility, and with bilateral cryptorchidism, leads to infertility. Even if one testicle is in place, its functioning is limited (antibodies are produced due to rejection of the undescended testicle).
Cryptorchidism in men is dangerous due to the risk of cancer, especially if the testicles are located in the abdominal cavity.
Symptoms of the disease are most pronounced and noticeable during puberty. Due to insufficient testosterone production, cryptorchidism in adolescents causes a tendency to become overweight.
Secondary sexual characteristics appear very slowly: hair on the face, in the axillary area and on the pubis grows weakly, and there is no loss of voice. In this case, the body constitution of boys is closer to a woman’s than to a man’s.
In addition, an inguinal or umbilical hernia may occur. Testicular torsion occurs much more often.
An important factor is the psychological discomfort of a teenager caused by his non-compliance with generally accepted norms.
Diagnosis of cryptorchidism
Cryptorchidism is initially diagnosed in the prenatal period. A pregnant woman undergoes an ultrasound, and if the testicle is undescended, scrotal asymmetry becomes noticeable.
In the first days of a baby's life, healthcare workers perform manual examination. Its important conditions are a warm room and warm hands of the doctor (otherwise a reflex muscle contraction is possible). If one or both testicles are not observed when palpating the scrotum, the doctor determines their possible palpation in the inguinal canal.
If the testicle is palpable, an attempt is made to bring it down into the scrotum. If the testicle remains in the scrotum for some time after being brought down, false cryptorchidism is diagnosed. Accordingly, if the testicle cannot be placed in the scrotum, or it immediately returns to its original position, true cryptorchidism is confirmed.
If the testicle cannot be felt, an ultrasound or MRI is performed. Based on the results of the study and the absence of a testicle, certain hormones are introduced, and if testosterone production does not increase in response, anorchism (absence of testicles) or monorchism (absence of one of the testicles) is diagnosed. Sometimes vasography with the introduction of a contrast agent is performed to confirm these diagnoses.
Treatment of cryptorchidism
There are two main ways to treat cryptorchidism:
- hormone therapy;
- surgical intervention.
To avoid testicular atrophy and cessation of sperm production, treatment with hormonal drugs is carried out. Human chorionic gonadotropin or male sex hormones are administered.
Conservative therapy is effective mainly if the testicles are not very high. It has some side effects, especially with large doses of drugs.
For example, hair may appear in the groin area or under the arms, the penis becomes enlarged, and the scrotum may become wrinkled.
If during the first year of life, as well as after a course of hormonal therapy, the testicle does not descend on its own, the only option is surgery. If it is carried out for 12 to 24 months, it is almost always possible to maintain fertile function.
There are exceptions when the operation has to be performed on a boy under the age of 1 year. It is necessary when the testicles are located very high.
The operation lasts on average 1.5 hours. The testicle is surgically removed from the groin area and placed into the scrotum through a previously made incision.
At the same time, the inguinal hernia, which often accompanies cryptorchidism, is removed; treatment with this method usually has no side effects, ensures normal development of the testicle, and reduces the risk of torsion.
If the testicle is located very high, the laparoscopy method is used.
The operation is difficult to perform, taking into account certain characteristics and age of the patient. Patients tolerate it well. After orchiopexy, you will only need pain relief and specialist supervision. For a month you need to avoid strong physical activity and sudden movements. During the operation, local anesthesia and sedatives are used as anesthesia.
Prognosis of cryptorchidism
The prognosis for cryptorchidism directly depends on the location of the testicles. The higher they are in the abdominal cavity, the faster changes begin to occur. If the testicles are localized in the lower part of the inguinal canal, there is a chance of their independent relegation.
If this did not happen in the first 12 months of life, or if the testicles are highly localized, surgical intervention is indicated. If the operation is performed in a timely and correct manner, the risk of loss of fertile function and the occurrence of cancer is practically reduced to zero.
In cases where surgery to solve the problem of congenital cryptorchidism was not used at an early age, the ability to procreate often cannot be restored.
Source: https://www.mosmedportal.ru/illness/kriptorkhizm/