- Genital warts are a disease of the genital tract, which is characterized by the appearance of warts in the vagina.
- And also in the area of the external genitalia - near the vagina, around the anus, sometimes on the inner thigh.
- Warts around the vagina and on its walls
- are a consequence of infection with papillomavirus (HPV infection).
- The human papillomavirus that has entered the body may not show itself for a long time.
- And only under certain conditions can its active reproduction begin.
- Among these conditions:
- infectious diseases of the genital tract – vagina, uterus, appendages
- frequent stress, climate change, obsession with mono-diets
- weakening of immune defense due to chronic general diseases
Warts occur together with vaginal candidiasis
Often, warts occur together with vaginal candidiasis (fungal infection) or against the background of other infections (chlamydia, ureaplasmosis, trichomoniasis).
What do viral warts look like near the vagina?
Genital warts are formations of small sizes (from 0.5 to 10 mm).
- The color of which, as a rule, does not differ from the color of the skin.
- If warts are located near the vaginal opening or on its walls, they may become injured during sexual intercourse.
- In this case, the formations may have a brighter color.
- Warts are usually painless.
- But, with an intravaginal location, they can cause discomfort during sexual intercourse.
- Condylomas are located singly or in small groups.
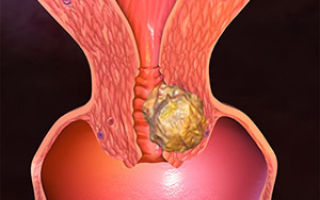
- Sometimes they merge and form conglomerates that resemble cauliflower in appearance.
Complications of warts in the vagina:
- 1. their injury
- 2.infection (inflammation)
- 3.ulceration
- 4. bleeding (in case of injuries)
- Also, warts in the vagina are dangerous for pregnant women, as they can infect the baby during childbirth.
- Vaginal warts are not just a cosmetic defect.
- Some subtypes of papillomavirus, leading to the occurrence of condylomas, can cause malignant lesions of the cervix.
- That is why, if there are warts in the vaginal area, they are not only removed, but also antiviral treatment is mandatory.
- Warts in the vagina: incubation period
- Women may encounter the first signs of condyloma formation quite often.
- The incubation period of warts in the vagina depends on the reactivity of the body.
- It can range from a couple of months to several years.
- In this case, visual manifestations may not be observed until the level of immunity in the body decreases.
- In most cases, the disease is asymptomatic.
Important! The first stages of development of formations do not cause discomfort in a woman.
- Even in the case of obvious presence of warts in the vagina, their carrier does not experience pain.
- How to recognize warts on women's genitals
- Warts visually appear as growths.
- Their sizes can be different: there are small formations and giant ones.
- They appear on:
- 1.labia
- 2. vaginal mucosa
- 3.cervix
- 4. pubic area
- 5.clitoris
- 6.around the anus
These formations may look different.
It all depends on the location:
- on the labia they are flat, flesh-colored, and crusty
- on mucous membranes, warts are soft, pink, flat with raised areas
- The formations can form groups that visually resemble cauliflower.
- Warts in the vagina: giant
- The size of ordinary condylomas is small (about 10 - 80 mm).
- Their shape resembles the comb of a rooster, and can be pointed or cauliflower-shaped.
- In case of hormonal imbalances or other changes in the body, warts can increase significantly.
- Such warts in the vagina are called giant warts.
- They lead to physiological discomfort, can bleed and cause pain.
- They reduce the wearer’s self-esteem and level of psychological comfort.
- If large formations are detected, they are removed.
- The optimal solution would be to conduct a histological examination of such a formation.
- Vaginal candidiasis and warts
- Vaginal candidiasis is an infectious disease that develops in the vaginal mucosa and often spreads to the uterus and the area of the external labia.
- The causative agent of the phenomenon is the Candida fungus.
- When the level of the body’s natural resistance (immunity) decreases, this type of fungus begins to actively develop
- Often, this disease is concomitant with warts in intimate areas.
- In this case, in addition to removing the formations, the doctor will prescribe antifungal therapy.
- Warts in the vagina with HIV: features
- In the case of HIV carriage, patients experience disruption of all functional systems of the body.
- Bacteria, viruses and other pathogens of inflammatory processes become more active against the background of suppressed immunity.
- Warts in the vagina with HIV manifest themselves in the active phase of the disease.
- When treating such formations, one should take into account the immune status and the degree of damage to the body's defense system.
- The course of treatment is usually prescribed after consultation with an immunologist.
Source: https://kvd-moskva.ru/virus-papillomy-cheloveka/708/
Warts in the vagina: causes and danger of the disease
The appearance of various growths on a woman’s genitals indicates the activity of the papillomavirus. The neoplasms are called warts, papillomas or genital warts.
Warts in the vagina or external genitalia may be harmless, but they cause discomfort for women, and if left untreated, the altered epithelial cells can develop into cancer.
What is this
The growths occur as a result of the multiplication of the papilloma virus in the basal layer of the skin or mucous membranes. As a result, the tissues are modified, turning into outgrowths with pointed tops.
At the initial stage of the disease, they are single formations, but as the disease develops, their number increases, and condylomas become outwardly similar to cauliflower or cockscombs.
Warts occur inside the reproductive system: in the vagina and on the cervix, and outside they affect the labia, clitoris and anus.
Depending on the characteristics of the neoplasms, two forms of the disease are diagnosed:
- exophytic - pathology is localized in the outer skin or mucous membranes;
- endophytic - a neoplasm develops in the thickness of the membranes of the vagina or cervix, often characterized by a malignant modification.
How do they manifest themselves?
At the onset of the disease, papillomas do not manifest themselves in any way and can remain undetected for a long time. When there are many of them, the symptoms acquire certain features that make it possible to detect the disease. The disease usually manifests itself as unpleasant sensations that occur after sexual intercourse.
This is because the condylomas can become injured, leading to pain and a burning sensation. In addition, slight bleeding after sex suggests the presence of neoplasms. In the later stages of the development of the disease, an unpleasant-smelling liquid may be released from the base of condylomas.
The discharge contributes to irritation of the mucous membranes, causing itching and burning, and damaged formations are dangerous due to the penetration of pathogenic microorganisms, which aggravate the symptoms by secondary infection. On the labia and in the vestibule of the vagina, growths are easy to detect on your own.
During hygiene procedures, a woman can feel sharp tubercles. Papillomas in the vagina can only be seen by a doctor during a visual examination. On the external genitalia, the growths appear as white hairs, and warts in the vagina are usually pink or red in color.
Genital warts or warts occur as a result of a woman being infected with the human papillomavirus. This infectious agent is in most cases transmitted through sexual contact of any form.
Less commonly, it can be contracted through personal hygiene items, for example, by using a towel from a person who is a carrier of the infection. The virus can exist in the external environment for some time.
Baths, showers or swimming pools are places that promote the spread of papillomavirus. A sick pregnant woman during childbirth transmits the virus to the child as it passes through the birth canal. After infection, the viral agent can remain latent for a long time. The impetus for the activation of the virus is a weakening of the immune system.
Factors causing warts in the vagina can be:
- vaginal microflora disorders, candidiasis;
- inflammatory processes in the organs of the reproductive system;
- chronic diseases;
- infectious diseases, frequent colds;
- hormonal disorders;
- intoxication of the body with drugs or alcohol;
- stress, overwork and other similar factors that suppress the immune system.
Warts in the vagina are caused by different groups of HPV. If the virus has a low degree of oncogenicity, then the pathological formations are benign and only cause slight discomfort.
Oncogenic viruses of the sixteenth and eighteenth types are quite common when affecting the membranes of the genital organs.
They are able to quickly lead the altered epithelium to the process of malignancy - degeneration into cancer cells.
If benign formations are not treated, then eventually oncology will develop even in cases where the warts are caused by the sixth or eleventh type of virus.
Transformation occurs when there are many papillomas and they are often injured. As a result, erosions occur, which lead to tissue inflammation and the degeneration of cells into a cancerous tumor.
Another danger is the addition of a secondary infection. Open wounds become entry points for various pathogenic microorganisms.
Thus, a woman begins to often suffer from genitourinary infections.
The presence of warts in the vagina poses a particular danger to the fetus. If a woman suffers from an illness during pregnancy, then the infection is likely to be transmitted to the child during childbirth. Before pregnancy, a woman should undergo an examination, and if growths are found, they should be removed and the infection treated.
Diagnostic methods
The doctor determines the disease based on a survey of the patient, a visual examination of the genital organs, and the results of cytological and histological examinations of the vaginal contents.
To more accurately identify the type of virus and determine the nature of the formations, a study is carried out using the polymerase chain reaction (CPR). The doctor carefully examines the vaginal cavity with a colposcope, identifying warts, the degree of development of the disease and possible associated infections. It also examines the external genitalia to identify foci of viral infection.
The results of laboratory tests show the nature of the tumors, the type of virus and the amount of antibodies to it, thanks to which the doctor can make a final diagnosis. Often, during the examination of the patient, sexually transmitted infections are detected. In this case, the woman is referred for examination to a dermovenerologist.
After making a diagnosis, the gynecologist prescribes appropriate treatment for the patient. Therapy for pathology caused by papillomavirus must be comprehensive.
In addition to antiviral drugs, immunomodulators that strengthen the immune system are prescribed, as well as medications that treat secondary infections.
Removal of papillomas in the vagina is required if the formations are large, occupy large areas or are cancerous.
Treatment with medications:
- Antiviral drugs that inhibit the development of HPV include Acyclovir, Viferon, Epigen-Intim and their analogues.
- You can normalize the function of the immune system with the help of Viferon or Cycloferon.
- Local cytotoxic drugs Vartek, Condilin or Podofilin will help stop the growth of the pathological formation.
- Warts are burned with solutions such as Solcoderm, Trichloroacetic acid, Condilox or Condilin.
Removal of papillomas in the vagina using hardware and surgical methods:
- Laser removal. The warts are melted by the laser beam. The method is considered quite reliable and rarely causes relapses.
- Radiosurgery. The safest way to deal with condylomas in the vagina and cervix. It is characterized by high accuracy, painlessness and absence of relapses, but is the most expensive method.
- Electrocoagulation. Allows you to remove growths using an electric current supplied at a certain frequency. The surgery may leave scars, and the procedure itself requires local anesthesia.
- Cryotherapy. The method of removing papillomas in the vagina is based on cauterizing the growths with liquid nitrogen. Does not require anesthesia, but can cause complications in the form of ulcers and bleeding wound surfaces.
- Surgical excision of papillomas is rarely performed, as it leads to severe bleeding from wounds and has a high risk of relapse.
Numerous folk recipes can be used as a supplement to the main treatment. Some of them are intended to treat external papillomas, while others help with growths in the vagina.
Condylomas localized on the labia can be treated with baths or compresses with medicinal plants.
Crushed fruits and horse chestnut leaves are perfect as raw materials for baths.
A compress of fresh Kalanchoe leaves will help you cope with warts located on the outside. Internal warts can be treated with decoctions that are introduced into the vagina by douching or tamponing. You can douche the vagina with decoctions of chamomile or St. John's wort. Aloe juice, which is soaked into tampons and inserted into the vagina for five hours, helps to cope well with the disease.
Therapy for pregnant women
Some drugs cannot be used by pregnant women, so treatment must be agreed with a doctor. Most often, she is prescribed immunostimulating drugs and topical medications, for example, Solcoderm. If removal of papillomas in the vagina is required, it is best to do this in the first trimester. In this case, radiosurgery will be the least dangerous option.
Prevention
In order to avoid an unpleasant disease, you should reduce the risk of infection through sexual contact. This will be possible in the absence of promiscuity or the use of contraception during sexual intercourse. It is also necessary to observe the rules of intimate hygiene.
If the virus is already present in the body, then in order for it to remain latent, it is necessary to maintain the state of the immune system at a high level. Infectious diseases of the genitourinary tract should not be allowed to progress to the chronic stage, otherwise, even after treatment, warts will appear again.
Source: https://med88.ru/papilloma/borodavki-vo-vlagalishhe/
Papillomas in the vagina: causes, symptoms and treatment
Proper care of intimate areas of the body involves not only hygiene procedures. Caring for the female genital organs means a correct lifestyle, since it is this part of the body that suffers the greatest number of various diseases. Most often, pathogens enter the female organs through sexual intercourse, so caring for intimate areas is also a protected intimate act.
A person can be a carrier of the papilloma virus for years and still not be aware of this fact. But one of the quite common problems is papillomas in intimate places, especially in the vagina.
Externally, such growths resemble small formations in the shape of a cockscomb or genital warts. Most often, the appearance of papillomas is caused by the papilloma virus. A healthy human body is capable of overcoming such formations on its own, if we exclude the influence of a number of provoking factors.
What is papilloma?
Often, papillomas look like small nodules that form in the vaginal area. They can acquire pigmentation from flesh to pink. There are both single specimens and several formations in one area. By merging with each other, they can form quite large clusters. If such a process develops, then we can talk about papillomatosis.
The emergence of such formations occurs under the influence of the human papillomavirus on the body. This pathogen is sexually transmitted and is quite common among the sexually active population.
In this article, we have already covered in detail the issue of human papillomavirus in women.
Why do vaginal papillomas occur?
Human papillomavirus infection has an incubation period ranging from 2 weeks to several years. Very often it causes the development of formations such as papillomas or condylomas in the vagina.
This pathogen enters the body through sexual intercourse and unprotected partners. The disease can develop against the background of reduced immunity or inflammatory processes.
Of particular importance is the presence of disease-provoking factors:
- endometritis;
- inflammation of the ovaries;
- vulvovaginitis;
- chlamydia;
- gonorrhea.
They lead to the rapid development of the virus inside the female body.
The development of papillomas in the vagina is also promoted by:
- early intimate life;
- avitaminosis;
- dysbiosis in the vagina;
- nervous shocks.
- decreased immune strength in the body;
- taking corticosteroids;
- performing surgical interventions on infected skin;
- pregnancy.
Papillomavirus has about a hundred different strains, of which only a few are capable of leading to the emergence and development of papillomas.
When the virus enters healthy tissue, a number of processes occur:
- The pathogen penetrates the basal layer of the dermis.
- Damages the cell membrane.
- Viral DNA is introduced into the center of the cell.
- The virus is waiting for favorable conditions.
If the carrier of the papilloma virus has a strong immune system, then the infection may not show its negative effects for a long time.
What do condylomas look like?
Quite often, the reason for visiting a gynecologist is the formation of condylomas on the intimate organs of women. Genital warts or condylomas are growths of the papillary epithelium, resulting in the formation of growths.
While condylomas are growing, the virus is not contagious. But as soon as the pathogen reaches the epidermis, there is a high risk of infecting its sexual partner.
There are two types of condylomas:
- Exophytic. The formations resemble genital warts in appearance. They are formed in the superficial layer and have a papillary surface. Such condylomas are provoked by HPV with low oncogenic activity. A photo of genital warts in women is presented here.
- Endophytic. They form flat condylomas. Very often they grow deep into the epithelium. Can provoke changes within healthy tissues. In the absence of timely treatment, they can cause oncological formations.
Condylomas can grow greatly, causing inconvenience:
- may bleed or be injured;
- interfere with intimate life;
- are in the nature of a cosmetic defect, while causing psychological discomfort;
- create problems during childbirth.
Photo
To understand the location and external signs of condylomas, use the photographic material provided below.
Symptoms of vaginal papilloma
Often, with HPV in women, the formation of papillomas is asymptomatic at first.
In case of prolonged development and progression of the disease, symptoms may appear:
- There is a feeling of itching and burning in the vagina.
- Bleeding may occur.
- Detection of growths in the vagina upon palpation.
Depending on the speed of development of the disease, a diagnostic examination of the patient will be necessary, followed by removal or treatment of the growths.
Diagnostics
To establish a diagnosis, a gynecologist needs a complete diagnosis:
- History of the disease. It includes knowledge of information:
- how long ago the growths appeared;
- whether there were unprotected intimate relationships;
- how long ago the last act of this kind took place.
- Examination by a gynecologist . In this case, the affected epithelial cells are collected for subsequent PCR analysis.
- PCR diagnostics. In this analysis, the number of pathogens and the type of papilloma viral infection are determined.
- Linked immunosorbent assay. It is necessary to confirm the presence of antibodies to the virus in a person. Based on which, one can judge the degree of development of HPV in the human body.
- Colposcopy. Inspection of the vaginal walls to determine damaged areas. It is carried out using a special colposcope device and staining the cervix with iodine solution.
- Anoscopy. Involves examining the anal area for the presence of papillomas.
- Cytological examination. Study of cells under a microscope, detection of damaged areas and their characteristics.
- Histological analysis. Studying the structure of damaged areas.
- Oncocytology. Study of cells in scrapings from the cervix and cervical canal under microscope magnification.
When papillomatosis is confirmed, timely treatment and correct selection of therapy are necessary.
Treatment of vaginal papilloma
Therapy for curing papillomas can be carried out in several approaches:
- Conservative treatment methods. Necessary to prevent the tumor from degenerating into a malignant formation. Includes purpose:
- Immunomodulators. They are used after testing the sensitivity of the papilloma virus to a specific medication. These include Viferon, Reaferon, Kipferon.
- Inducers of interferon production. Prescribed after determining the effect of such drugs on the affected areas. Representatives of drugs: Tamerit, Neovir, Larifan.
- Specific drugs that have an antiviral effect. Most often prescribed: alpirazine.
- Surgical techniques for the treatment of papillomas. Several types of formation removal are used:
- Chemical coagulation. Carry out under the influence of drugs: solkovagin, podophyllin.
- Cryodestruction. The procedure is effective for small affected areas.
- Electrocoagulation. It is carried out using a laser.
- Radio knife or excision with a scalpel. Prescribed only for extensive lesions.
Drug treatment
Very often, treatment of papilloma virus occurs under the influence of a whole range of medications.
They have the following properties:
- cauterizing;
- bactericidal;
- oppressive.
At the same time, their spectrum of action contains a component, the influence of which prevents the neoplasm from developing. The virus may be resistant to some antibiotics, so before prescribing treatment, it is advisable to identify the most effective ones.
The main means of fighting infection include:
- lapis pencil;
- drops;
- pills;
- ointments.
If removal of papillomas is not practical, then you can get rid of the growths in 2-3 weeks with the help of medications.
The following have a detrimental effect:
- Feresol.
- Phenol in glycerin solution.
- Super clean.
- Salicylic acid.
- Cryopharma.
In addition to the direct effect of solutions on papilloma, general-effect drugs are also used that increase the immunological status of the body.
Removal
Sometimes it is impossible to cure papilloma without removing the affected area.
Then they resort to the following procedures:
- Excision of formations. It is carried out in cases of large lesions of the skin.
- Treatment with chemical drugs that have a detrimental effect.
- Freezing the damaged area. It is possible to carry out this procedure in the vagina. The advantage of this manipulation is to control the effects of cold without touching healthy tissue.
- Use of chemical removal techniques.
Prevention
In order to avoid infection with the papilloma virus, you must adhere to a number of recommendations:
- Have regular examinations with a gynecologist.
- Maintain personal hygiene.
- Allow unprotected intimate contact only with trusted partners.
- Boosting immunity.
- Balance your diet.
- Get tested for the presence of HPV in your body once a year.
- Rejection of bad habits.
The danger of self-removal of papillomas in the vagina
Papillomas can provoke the development of diseases:
- Erosion of the cervix.
- Dysplasia.
- Go to malignant formations.
If the formation is injured by:
- squeezing;
- friction;
- integrity violations;
- unprofessional or self-removal of papillomas.
Possible consequences include the degeneration of a benign formation into an inflammatory process with a high oncogenic risk. Therefore, self-treatment or removal of papillomas from the vagina is simply unacceptable.
Conclusion
Papillomas are very insidious. They can spread quickly and cause harm to the entire body. When papilloma appears, it is necessary to consult a doctor, as they can degenerate into oncological formations.
By following several preventive recommendations, it is possible not only to protect yourself from papillomas, but also to prevent the pathogen from entering the body:
- Protect yourself with condoms during intimate intercourse.
- Avoid stressful situations.
- Strengthen your immune system.
- Get checked by your doctor promptly.
Strong immunity can protect a woman from the appearance of papillomas for a fairly long period. Even if the virus enters the body of a healthy person, its development will be suppressed by the body’s immune forces.
Material updated: 04/01/2019
Source: https://heal-skin.com/novoobrazovaniya/papillomy/papillomy-vlagalishha.html
Warts on the labia and vagina: causes and treatment
The appearance of intimate warts is a very unpleasant discovery in a woman’s life, causing a feeling of self-doubt and stiffness in movements. But it is not so. The appearance of skin growths indicates the onset of an infectious disease. Therefore, warts on the labia require serious attention and treatment.
Types and localization of warts
Skin tumors that grow on the mucous membrane of the genital organs or on the labia majora are also called papillomas. They are divided into two types:
- flat papilloma (dense, flat, difficult to notice growth, slightly rising above the surface of the skin);
- condyloma acuminata (papillary-shaped soft growth on a stalk, narrowed in the upper part).
The locations of flat papillomas and genital warts are very different. They appear as warts in the vagina, on the labia, on the inside of the upper thigh, around and inside the anus. Flat papilloma near the vagina and on the cervix is considered the most dangerous, as it can develop into cancer.
Reasons for appearance
The development of papillomas on the labia indicates the activation of HPV in a woman’s body. Papilloma viruses types 6, 11, 16, 18 are the cause of warts in the intimate area.
After entering the body, the virus is able to remain unnoticed for some time, without giving itself away. The immune system also plays an important role here, thanks to which the woman does not experience any discomfort for several months or even years.
A wart that appears in the vagina or on neighboring organs means a decline in the immune system, which has failed to cope with its protective function. When a virus enters a cell, it reprograms it by inserting its DNA into the cell's DNA. As a result, excessive division occurs and a wart is formed.
How does infection occur?
Genital warts are transmitted primarily through sexual contact. Most often, infection occurs during sexual intercourse without the use of barrier methods of contraception. But a condom does not provide 100% protection against infection, since it does not cover the entire surface of the contacting skin.
There is a possibility of infection in other ways:
- through the use of shared towels or other personal hygiene items;
- wearing someone else's underwear;
- contact with surfaces where a sick person was in a sauna or swimming pool.
For the virus to enter the body, its presence in the external environment and even a small injury or crack on the surface of the skin is sufficient.
Risk factors
The risk group for the appearance of warts on the surface of the skin of the genital organs, as well as in the vagina, includes women:
- those who started sexual activity early;
- having an infected partner and not using barrier contraceptives;
- having multiple sexual partners;
- a permanent partner of whom has several partners.
The virus may be present on the skin and mucous membranes of men without showing any external signs of its presence, but the infection is transmitted through sexual contact.
What is the danger
Vaginal warts grow under the influence of several strains of HPV. They are divided into:
- non-oncogenic;
- oncogenic medium risk;
- high-risk oncogenic.
The last group includes the sixteenth and eighteenth HPV strains. Growths caused by these types of viruses, without proper treatment, in 90% of cases lead to cancer of the cervix and other organs of the female reproductive system.
If you notice the first signs of HPV, we recommend that you immediately consult a doctor.
Flat formations can go unnoticed for a long time, especially when localized on internal organs. They can only be detected during a medical examination, so it is highly recommended to visit a gynecologist regularly.
Diagnostics
The appearance of a wart on the labia may not be the only symptom of an infection. The presence of nodules inside the cervical canal can be suspected by the appearance of a feeling of itching or burning, slight bleeding accompanying sexual intercourse, which is associated with injury to the growth. These are clear signals to contact a doctor.
After a visual examination, the specialist performs a colposcopy - a visual examination of the vagina and cervix with the ability to enlarge the image, take smears or tissue for further examination. The resulting biological material is sent for PCR diagnostics, which makes it possible to determine the specific strain of the virus and its quantity in the source of infection.
If necessary, additional cytological and histological studies are carried out to determine the state of the immune system.
Treatment
The treatment of warts on the labia requires an integrated approach. The goal is not only to get rid of the skin growth, but also to overcome the infection, strengthen the immune system in order to maximally protect the body from infections in the future and minimize possible relapses.
Local medications
Warts on the labia majora or surrounding external tissues are treated using external agents in the form of ointment, spray or gel with antiviral and immunostimulating effects: Panavir, Viferon.
To combat condylomas inside the vagina, vaginal suppositories are prescribed. Most often these are drugs based on interferon or those that promote its production: Laferobion, Altevir, Proteflazid.
Antiviral agents for oral administration
Antiviral tablets and injections have been developed to treat this sexually transmitted infection. Most antiviral drugs also have immunomodulatory properties: Isoprinosine, Alpizarin, Cycloferon.
Radical techniques
- If the patient’s condition is advanced, the tumors have grown significantly, threaten to develop into oncology, or there is another important reason, the doctor prescribes removal of the papillomas.
- Medical and cosmetology institutions offer various procedures and operations for removal:
- Cryodestruction. Using a special apparatus and a correctly sized nozzle, a specialist acts on the papilloma with liquid nitrogen at a temperature of minus 190 degrees. The growth freezes and disappears after a few days. The procedure is painless in most cases due to the low temperature.
- Laser burning. The laser beam is directed selectively at the growth and evaporates it. The advantage of the method is the accuracy of the impact. After the procedure, a scab forms, which falls off on its own after a few days. As in the case of cryodestruction, you should never try to remove the scab yourself.
- Electrocoagulation. The ability to select the optimal nozzle also increases the effectiveness of the procedure. For example, if the growth has a leg, it can simply be cut off with an electric loop, cauterizing and disinfecting the remaining tissue, which at the same time prevents bleeding.
- Chemical cauterization involves the use of various acids that destroy papilloma. Requires increased attention, as there is a possibility of damage to healthy tissue.
- Surgical excision. It is used only if it is impossible to remove the papilloma in any other way, in case of large growths or cancerous degeneration. In the latter case, a larger area is captured, deeper layers of skin are cut out, and a scar remains after the operation.
Traditional medicine
When it comes to removing papilloma, traditional medicine offers its own methods: using garlic juice, apple cider vinegar, celandine, and hydrogen peroxide. They are good for removing growths of less delicate localization.
But when it comes to treating vaginal warts, such remedies may not only be unavailable (for technical reasons), but also cause a burn to the mucous membrane and delay the treatment of a dangerous infection. Therefore, experts urge you not to self-medicate in this area.
Causes of appearance and methods of treatment in children
The appearance of papillomas on the genitals in children can be caused by several reasons:
- Infection during childbirth from the mother. The infection is not transmitted in utero, but during passage through the birth canal.
- Through the use of common household and hygiene items with infected family members (towel, bathtub, toilet) or in a public place.
In addition, there are other skin diseases that are important not to be confused with papillomatosis: molluscum contagiosum, lichen planus.
In any case, the appearance of skin formations in a child indicates a weak immune system. It is necessary to consult a doctor as soon as possible to agree on a further plan of action.
Treatment prognosis
With a timely reaction and a qualified approach, the disease can quickly be transferred to a latent state, but one should not forget about it. It is impossible to completely remove the infection from the body. This means that if unfavorable factors occur, warts will appear again.
However, in medical practice, cases of complete recovery from infection within one year have been observed. Therefore, you never need to despair, you just need to keep your body healthy.
Disease prevention
Prevention is directly related to awareness of the dangers of the disease and how it is transmitted. Several categories can be distinguished:
- Since the virus can enter the human body primarily through sexual contact, it is important to inquire in a timely manner about the health status of your partner and, if necessary, undergo diagnostics and treatment together. Casual connections should be avoided.
- Pay attention to intimate hygiene, use exclusively your own accessories, even with your family, and adhere to general sanitation rules.
- Takes care of physical and mental health: mental work, physical exercise and rest must be balanced.
- Women are advised to regularly visit a gynecologist to detect the disease in the early stages.
As a preventative measure, vaccination against HPV is carried out with Gardasil or Cervarix. Teenage girls should be vaccinated before they become sexually active. After administering a three-time dose, 100% protection against the most dangerous strains of the virus is guaranteed.
Source: https://SkinPerfect.ru/borodavki/vaginalnye
Benign tumors of the vagina
Update date: 05/14/2019
Benign vaginal tumors are neoplasms that form from cells of connective, adipose and epithelial tissues together with blood vessels. Non-malignant formations, which are either a single nodule on a wide base or on a long stalk, or multiple nodules (rare), are usually localized under the mucous membrane of the vaginal walls.
Benign tumors in the vagina exhibit slow growth and a compressive effect on the surrounding tissue structures, but do not grow into them, do not metastasize or recur. Such neoplasms most often affect women aged 20 to 50 years.
Benign tumors of the vagina - fibroids, fibromas, myxomas, hemangiomas, lipomas and papillomas - occur with varying frequency.
Myomas, fibroids (or fibromyomas), and rarely vaginal lipomas are benign tumors that form from cellular growths of smooth muscle, connective or adipose tissue.
They have sharply limited round or oval contours, smooth relief, dense or soft consistency (depending on the histological structure), limited mobility and painless connection with the submucosal layer of the vagina or with the thickness of the labia majora.
Hemangiomas are vascular tumors of the vagina in the form of red-purple or bluish spots rising above the mucous membrane, having a soft consistency, capillary and cavernous structure.
The surrounding mucosa is swollen, the folds are compacted, the epithelium is loose. From localization in the submucous membrane of the vagina, hemangiomas can expand towards the cervical canal and even into the uterine cavity.
Ulceration and necrosis of these neoplasms often occurs.
Lipoma develops from mature adipose tissue in the pubic area and labia majora in the form of a fat capsule. The tumor has a soft consistency - mobile, with a clearly defined shape.
Myxoma is a tumor that forms from the remains of embryonic connective tissue. It occurs mainly in older women with localization in the subcutaneous fatty tissue of the pubis and labia majora. It is characterized by slow growth and is not prone to malignancy.
Papillomas (condylomas) are non-cancerous epithelial tumors, in the form of papillary “placers” on a wide base or on a thin stalk on the walls of the vagina. Their appearance signals the presence of a common papillovirus infection in the body.
Lymphangioma develops from lymphatic vessels, usually located near the inguinal folds.
This is a multiple small-lumpy benign tumor, formed as a result of the fusion of a large number of nodules, consisting of cavities of different shapes and sizes containing lymph. The walls of the cavities are formed by connective tissue and lined with endothelium.
The appearance of soft lymphangioma is characterized by a swelling of a pale bluish color, slightly tender or painful. In addition, the tumor may have dense inclusions and sometimes suppurate.
Cysts are much more common in the vagina. By the way, Bartholin gland cysts are many times more common than all benign tumors combined, with the exception of papillomas localized on any layer of the skin.
Often, retention cysts form in the upper part of the vagina on the right or left wall, which are residual formations of the early intrauterine period. The embryo initially develops both the Wolffian (Gartner) duct and the Müller duct.
In the process of further development of the fetus, male genital organs are formed from the right and left Wolffian ducts, and female genitalia develop from the right and left Müllerian ducts. Then the duct left without use dies, however, the remnants of both systems of passages can degenerate (more often in young women) into cysts.
The same cysts can sometimes form from atypical focal inclusions from the epithelial layer in the thickness of the vaginal wall or in former hematomas.
Prognosis for benign vaginal tumors
Despite the fact that benign vaginal tumors rarely transform into malignant ones, it is considered best to remove them by any suitable method without involving healthy tissue. Relapses are extremely rare. It is important to monitor your health, detect tumors in time and radically get rid of them.
The asymptomatic existence of benign vaginal tumors lasts until their increased size begins to manifest itself with various disorders:
- sensation of a foreign object in the vagina;
- feeling of discomfort during sexual intercourse;
- disturbances in the process of defecation;
- itching, burning sensation in the vagina due to papillomas;
- unusual discharge;
- inflammation, suppuration, necrotization in cases of hemorrhage into the tissue of the neoplasm or when its legs are twisted;
- malignancy of the tumor - extremely rare;
- nagging or contact pain;
- changes in the act of urination;
- swelling of the adjacent mucosa;
- looseness of the covering epithelium;
- thickening of folds;
- heavy and prolonged menstrual bleeding (with deep hemangiomas).
Diagnosis of benign vaginal tumors is carried out in several ways, depending on its type and location.
Gynecological examination. In the speculum, a tumor node with a wide base or on a stalk in the submucosa of the anterior vaginal wall, up to the size of a chicken egg, is visualized.
A hemangioma appears as a raised red, purple, or bluish patch surrounded by loose, swollen mucosa and thickened folds.
Bimanual examination makes it possible to palpate a dense, formed tumor, inactively associated with the wall of the vaginal cavity.
- Colposcopy reveals a wide network of unstable blood flow paths with varicose changes in blood vessels with hemangioma; it is required in the presence of all types of vaginal tumors, especially with papillomas, and for taking smears and parts of the affected tissue for histological examination.
- Transvaginal ultrasound shows an extensive picture of the presence and structure of any vaginal tumors according to the degree of their echogenicity.
- Cytological examination of the smear and PCR analysis of the smear to determine the papilloma virus (HPV), which has a high oncogenic risk, and the liquid cytology method will give more accurate results.
- Histological examination must be used to study removed benign tumors.
Vascular tumors that do not undergo any changes, do not increase in size and do not disrupt the normal functioning of the woman’s genital organs for a long time require only regular medical supervision.
Treatment of non-malignant vaginal tumors can be medicinal and surgical:
- treatment with Solkovagin is used for papillomas;
- excision or desquamation of a formation from the vaginal submucosa, intersection and ligation of the pedicle;
- if there is a threat of injury to nearby organs of the urinary system and rectum, partial excision of the cyst wall is possible with ligation of the edges and drainage of the resulting cavity;
- cryotherapy - tumor removal with liquid nitrogen;
- electro- or plasma coagulation—cauterization or evaporation of the tumor and blood vessels;
- sclerotherapy - injections of special drugs that stop blood vessels;
- removal of the tumor simply with a scalpel, laser or a targeted beam of high-frequency radio waves (radio wave therapy).
After each treatment procedure, appropriate medication support and a gentle regime are required for a period of time determined in each individual case by the doctor.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice. Consult your doctor for diagnosis and treatment.
Still have questions?
Enter your information and our specialists will contact you and provide free advice on issues that concern you.
Source: https://www.medcentrservis.ru/disease/dobrokachestvennye-opuholi-vlagalishcha/
Benign tumors of the vagina
Of the benign tumors of the vagina, clinical gynecology encounters cysts, fibroids, myomas, lipomas, papillomas, and hemangiomas.
The origin of benign vaginal tumors is polyetiological; in their development, a certain role is assumed to be disorders of neuroendocrine regulation, exposure to viruses, and recurrent colpitis. Benign vaginal tumors are more often found in patients aged 20-50 years.
The need for surgical tactics in relation to vaginal tumors is dictated by the possibility of their suppuration, necrosis, and, less often, malignant degeneration.
Benign tumors of the vagina
True benign tumors of the vagina include fibroids, myomas, fibromyomas, and lipomas.
The growth of benign vaginal tumors is based on the proliferation of connective (fibroma), smooth muscle (fibroids), and less commonly adipose (lipoma) tissue.
True tumors are localized under the mucous membrane of the vaginal wall; may look like a single node with a wide base or a long stem; less often they are in the nature of multiple nodules.
Clinically, vaginal tumors can manifest themselves as nagging or contact pain, foreign body sensation, discomfort during sexual intercourse, and disturbances in defecation and urination. Torsion of the leg or hemorrhage in the vaginal tumor tissue may be accompanied by necrotization, inflammation or suppuration. In rare cases, malignancy of benign vaginal tumors is observed.
True vaginal tumors are detected during a gynecological examination. During bimanual examination, a tumor associated with the vaginal wall is palpated, having clear boundaries, dense consistency, and limited mobility.
When examined in the speculum, a node is found located in the area of the anterior wall, on a broad base or pedicle under the unchanged vaginal mucosa. The size of true vaginal tumors can reach a chicken egg.
During transvaginal ultrasound, a solid structure of vaginal tumors is visualized, with average or reduced echogenicity, similar to uterine fibroids.
For asymptomatic vaginal tumors, they can be monitored dynamically.
If there is a tendency to growth or clinical symptoms, vaginal tumors are removed surgically: they are peeled off from the submucosal layer within the bed or the stalk is cut off.
The operation is often performed through a transvaginal approach; Deeply located vaginal tumors can be removed using abdominal wall transsection. The morphological form of the vaginal tumor is determined during histological examination of the specimen.
Papillomas (condylomas) of the vagina
Papillomas (condylomas) are tumors of the integumentary epithelium that look like papillary growths on the vaginal mucosa. Papillomas are a manifestation of a common human papillomavirus infection.
They have exophytic growth, have a thin stalk or a wide base. Papillomas can manifest as itching, burning in the vagina, contact bleeding due to trauma, and unusual discharge.
Papillomatous tumors of the vagina in some cases undergo decay or malignancy.
Diagnosis of papillomas includes cytological examination of a smear, colposcopy, biopsy of a vaginal tumor with histological examination, PCR determination of HPV with typing of non-oncogenic and oncogenic strains.
Removal of vaginal papillomas is strictly necessary and can be done with medication, liquid nitrogen, laser, electrocoagulation, plasma coagulation, surgical scalpel, or radio wave method. After removal of papillomas, immunomodulatory therapy is prescribed.
Vaginal hemangioma
Hemangiomas are vascular tumors of the vagina with a soft consistency. Based on their structure, capillary and cavernous hemangiomas are distinguished. Having arisen on the vaginal mucosa, hemangiomas can spread to the cervical canal and into the uterine cavity. In some cases, ulceration and necrosis of vascular tumors of the vagina are noted.
Vaginal hemangiomas often manifest themselves as contact bleeding due to trauma. When a vascular tumor of the vagina spreads to the internal genitalia, a clinic of hyperpolymenorrhea may occur.
During a gynecological examination, a vaginal hemangioma appears as a red, purple or bluish spot rising above the mucosa. Local swelling of the mucous membrane, loosening of the integumentary epithelium, and engorgement of folds are noted. During colposcopy, attention is drawn to the presence of an extensive network of anastomosing, and in some areas, varicose vessels.
Non-progressive, non-ulcerating, vascular tumors of the vagina that do not disrupt the ovarian-menstrual cycle can be left under observation. With a progressive clinical picture, vaginal hemangiomas can be removed surgically, using cryotherapy, electrocoagulation, or sclerotherapy.
Despite the fact that malignancy of unresected benign vaginal tumors occurs infrequently, the optimal tactic for them is radical excision within the boundaries of unchanged tissue. Relapses after removal of vaginal tumors are rare.
The presence of a vaginal tumor is an aggravating factor in the course of pregnancy, since it can interfere with normal childbirth, provoke discoordinated labor, and bleeding. Management of pregnancy in women with a benign vaginal tumor requires dynamic monitoring of the condition of the tumor and early selection of the method of delivery.
Source: https://www.KrasotaiMedicina.ru/diseases/zabolevanija_gynaecology/vaginal-tumor