Age-related changes in a man’s body after 45-50 years can cause the development of prostate adenoma. In every fifth case, this disease is treated through surgery. We will talk about various methods of surgical treatment, their features and advantages today in our article.
Why is an adenoma dangerous?
At this stage, the man notices the first signs of the disease. The main ones are problems with urination: the number of urges increases, the outflow of urine worsens, and additional effort is required to empty the bladder.
Further development of the disease leads to stretching of the walls of the bladder and the formation of stagnation of urine, disruption of the kidneys, and general intoxication of the body.
In particularly advanced cases, the adenoma can completely block the urethra, causing acute urinary retention. At the very beginning of the development of hyperplasia, conservative treatment makes it possible to stop tissue growth.
At later stages, surgical treatment of prostate adenoma is used.
Indications for surgery
Immediate surgery is necessary in the following cases:
- traces of blood appeared in the urine;
- the patient has symptoms indicating impaired renal function and the development of urolithiasis;
- a large amount of residual urine accumulates in the bladder;
- the tumor blocked the urethra and caused complete urinary retention.
Operation methods
Modern medicine offers several types of operations to eliminate prostate hyperplasia. When choosing a method of surgical intervention, the patient’s age, his condition, the need to preserve sexual function and some other factors are taken into account.
The most commonly used:
- transurethral resection;
- open removal of the prostate;
- transurethral incision;
- removal of adenoma with laser.
TOUR
For resection of the prostate gland, a special medical instrument with a video camera is used, which allows all manipulations to be performed with maximum precision. The purpose of the operation is to cut off the part of the prostate that is compressing the urethra. The procedure is performed under general or local anesthesia. To prevent bleeding, the circumcised vessels are immediately cauterized. After the procedure is completed, a catheter is inserted into the urethra to drain urine and rinse the bladder.
TUR is recommended for patients who want to preserve sexual function. This type of surgical intervention is used when a malignant tumor is suspected. The average duration of the operation is 1 hour.
Open prostate removal
Manipulations are performed through an incision in the lower abdomen or perineum. The disadvantages of open adenoma removal include a long period of postoperative rehabilitation. The main advantage of this treatment method is the low relapse rate.
Prostate incision
The main complication of cutting the gland can be intense bleeding. If during the operation a large amount of blood enters the cavity, repeated intervention will be required.
When incising the prostate tissue, there is a high probability of developing such a postoperative complication as retrograde ejaculation (the release of seminal fluid occurs not into the urethra, but into the bladder). Therefore, the use of this method is not recommended for men who plan to have children in the future.
Removal of hyperplasia using laser
The use of a laser to eliminate overgrown prostate tissue allows you to return to your normal life within a few days. A significant advantage of the procedure is the minimal risk of negative consequences, including sexual dysfunction.
Removal of hyperplasia is carried out by two methods: with vaporization, the tissue is removed in layers, and with enucleation, evaporation occurs in small pieces. This allows you to examine the tumor formation and exclude its malignant nature. Thanks to the simultaneous removal of tissue and cauterization of the wound surface, the likelihood of bleeding is virtually eliminated.
Possible complications
With any operation there is a certain risk of complications. Surgical complications include bleeding, infection in the wound, and injury to nearby organs.
After the rehabilitation period, such negative consequences of surgical intervention may appear as retrograde ejaculation, absence of the urinary retention reflex, narrowing of the urethra, re-growth of hyperplasia, and impaired erectile function.
Postoperative rehabilitation
To prevent the development of inflammatory processes in the wound, antibacterial drugs are prescribed. The course of administration depends on the speed of healing of wound surfaces and the presence of complications. A catheter for urine removal can remain in the urethra for 3 to 10 days.
The total length of the recovery period depends on the method of surgery.
To prevent possible complications and rapid healing of wounds during rehabilitation, the following rules should be followed:
- You should not make sudden movements, engage in heavy physical labor, or lift weights;
- it is necessary to monitor the digestion process and avoid constipation;
- you should abstain from sexual intercourse for 1.5-2 months;
- For timely detection of complications, it is necessary to regularly visit your doctor.
Source: https://kaklechitprostatit.ru/lechenie/operativnoe-lechenie-adenomy.html
Surgery for prostate and adenoma in men: types of surgical treatment
If the treatment of prostatitis with traditional methods using medications, physiotherapeutic procedures and the use of traditional medicine did not achieve a positive result, then the doctor may recommend surgery to the patient. Its purpose is only to exclude the consequences and complications of the disease, which, as a rule, remains. Moreover, after surgical therapy, the symptoms of inflammation go away: urination problems and sexual dysfunction.
Prostatitis and methods of its treatment
The need for surgery does not occur often. Usually it is possible to defeat the disease without radical measures.
Prostatitis is a common disease of the genitourinary system of the stronger half of humanity, in which the prostate gland becomes inflamed. It can be triggered by infections or other factors, such as: decreased immunity, hypothermia, sedentary lifestyle, stress, irregular sex.
Two forms of the disease are diagnosed: acute or chronic prostatitis.
The first is rare, has an infectious nature of origin, and is characterized by a severe course with pronounced symptoms: severe pain in the pelvic region, fever, difficulty urinating, the presence of blood in the urine, pain during ejaculation. In these cases, emergency medical care with hospital treatment is needed.
The chronic form is common and is more difficult to detect due to subtle signs. The patient may suffer from pain in the lower abdomen, frequent urination, sexual dysfunction, and discharge from the urethra. There are also asymptomatic cases of the disease; in such cases, the fact of pathology is established only by the results of tests.
Medicine today has a variety of methods for treating the disease. The choice depends on its form, duration, presence of complications and characteristics of the patient’s body.
Treatment is carried out on an outpatient basis or in a hospital. The patient first undergoes the necessary examination and tests, based on the results of which appropriate therapy is prescribed.
Important! Prostatitis can only be cured using several methods in combination.
Drug therapy
Drug therapy for prostatitis consists of taking the following groups of drugs:
- antibiotic;
- painkillers;
- alpha blockers.
Surgical intervention
Surgical treatment of prostatitis in men has been carried out for a long time, but in recent years the attitude towards this method has changed in favor of less radical interventions.
Transurethral resection (TUR)
The essence of the operation is as follows: to reduce the pressure on the urethra, the entire prostate gland or part of it is removed. The operation is performed in a “closed” way, using a resectoscope, which reduces the likelihood of complications. As a result, signs of inflammation and pain go away.
Prostatectomy (adenectomy)
The prostate is removed during a routine “open” operation. The recovery period in this case is much longer than with TUR. But sometimes only this method can help.
Non-surgical treatment methods
With the development of technology, minimally invasive treatment methods are becoming more and more popular. They are recognized as more effective and gentle.
- Thermal methods. The most commonly used method is transurethal microwave thermotherapy. A positive result is achieved by exposing the affected area to elevated temperatures.
- Ultrasound. According to reviews, this is one of the most effective methods of treatment. The effect is obtained using ultrasonic waves. The procedure is painless.
- Cryodestruction. Using liquid nitrogen, diseased tissue is removed.
- Laser methods. Used in case of chronic prostatitis. Under the influence of laser beams, the body's defenses and tissue regeneration are mobilized.
- Magnetic laser inductotherapy. Simultaneous exposure to a magnet and laser improves blood circulation, relieves pain, stimulates healing, and enhances the effect of medications.
- Balloon dilatation of the urethra. The urethra is mechanically dilated by inserting a catheter ending in an inflatable balloon.
- The stenting method involves increasing the diameter of the urethra using a stent – a cylindrical formation made of polymers.
- Massage is used in conjunction with other techniques. It improves blood circulation in the prostate and relieves congestion.
- Hirudotherapy. The use of leeches in the treatment of prostatitis increases the flow of lymph and blood to the gland, improving its function.
Surgical methods for treating prostate adenoma are mostly the same as for inflammation.
Surgery for prostatitis
In case of chronic or non-bacterial prostatitis, surgery is the last resort. Indications for surgical treatment are complications such as:
- acute urinary retention;
- negative results of treatment with conservative methods;
- constant presence of blood in the urine;
- stones in one of the organs of the genitourinary system, which appeared due to urination problems;
- frequent infectious diseases of the urinary system;
- purulent discharge;
- paraproctitis.
But there is a certain list of contraindications under which prostate surgery is strictly prohibited:
- acute inflammation in the genitourinary system;
- patient over 70 years old;
- diabetic disease;
- ARVI;
- Diseases of the cardiovascular or respiratory system;
- hemophilia;
- taking anticoagulants;
- hyperthyroidism.
Surgery for prostatitis is a non-standard treatment method. They are forced to resort to it when all other methods have been tried.
Types of surgical treatment
When choosing a method of surgical intervention, the patient’s condition and the presence of concomitant diseases are assessed. Preference, whenever possible, is given to low-traumatic methods.
Prostatectomy
The gland is completely removed. According to the method of implementation, there are two types:
- Abdominal (invasive) surgery. The surgeon makes an incision between the anus and the scrotum. The gland is removed using a resector.
- Endoscopic procedure. It is carried out through punctures in the wall of the abdominal cavity.
Cavitary prostatectomy is rarely done. The surgeon, first of all, needs to preserve the nerve endings to maintain erectile function.
Transurethral resection (TUR)
The prostate is removed through the urethral canal using a resectoscope. TUR is considered a low-traumatic method, but there are conditions regarding the amount of gland to be removed.
Laparoscopy
The procedure is performed through small punctures in the walls of the abdominal cavity. A special resectoscope guided by ultrasound is used to remove the inflamed part of the prostate in men; This operation is characterized by low blood loss, precise sections and a short recovery period.
Laser removal of prostatitis
Laser removal of the prostate gland is a very effective method of combating prostatitis and adenoma. One disadvantage is the high cost of the operation. Using a laser, you can remove inflamed tissue, cope with spasms, adhesions and scars, eliminate the causes of the disease, and normalize urination. The recovery period is minimal.
Abscess drainage
Used for purulent prostatitis. A puncture needle is used to rinse the inflamed tissues with a disinfectant solution through a puncture. To facilitate urination, drainage is installed in the urinary canal. The patient wears a urine bag until the process of urine outflow is restored.
Preparing the patient for surgery
To reduce the risk of complications in the postoperative period, careful preparation for the surgical procedure is required.
- The patient undergoes a complete examination. The method and its possible complications are discussed with the attending physician.
- Taking into account the patient’s health condition, based on examination data and test results, the anesthesiologist selects drugs for anesthesia.
- The doctor explains in detail the consequences of the operation, and the limitations are specified. Sexual activity after the procedure can be resumed only when the surgical wound has completely healed, in order to avoid bleeding.
- 7 days before surgery, a course of antibiotics and hemostatic drugs begins. The use of anticoagulants is temporarily suspended.
2 days before surgery, the patient is prescribed plenty of fluids. It is recommended to give up cigarettes and alcoholic beverages.
Rehabilitation period
Successful surgical treatment of prostate inflammation depends not only on the correct operation. Postoperative therapy is of great importance. Immediately after the intervention, the patient is given plenty of fluids to remove blood clots from the urethra. Local anesthetics are used for pain relief. Adhere to the general rules of conduct during the rehabilitation period:
- A weekly course of antibiotics is prescribed to prevent infection. Decongestant drugs are also prescribed to normalize prostate activity and prevent relapses. In cases of dysuretic disorders, the patient is given drainage for the time necessary to restore normal urination. Next, it is recommended to wear diapers, which help with involuntary urine discharge.
- In the following months, the patient undergoes courses of physiotherapy and exercise therapy, which helps restore urinary and erectile function.
Patients who have undergone surgery on the prostate gland are given the following mandatory recommendations:
- When playing sports, it is recommended to avoid heavy loads on the pelvic area.
- They advise you to change your habits: they recommend switching to crushed food, drinking up to 3-5 liters of liquid per day, eliminating fatty, smoked foods, and not drinking canned food or alcoholic beverages. No smoking.
- Sexual life can begin only after the organ has healed. Having sex is an excellent prevention of prostatitis.
Consequences of the operation
It is known that surgery does not eliminate prostatitis, but only relieves the signs of the disease: urination disorder, pain.
Therefore, such interventions are resorted to as a last resort. But no one is immune from complications after surgery. There are:
- Relapse of the disease. After treatment of the prostate through surgery, the inflammatory process may recur. Prostatitis appears secondarily after surgery in 10-15% of patients. The patient should know the symptoms of an exacerbation and immediately go to the doctor. Pain occurs during urination and sex, and body temperature rises.
- Adhesions may form. This is dangerous for the development of infertility.
- Bleeding occurs most often. Abundant losses are compensated for by transfusion, and in case of light bleeding, saline solutions are administered.
- Water intoxication. The cause is moisture entering the blood. This occurs during the process of washing the surgical field after resection of the prostate gland.
- Urinary disorders. Involuntary discharge or acute urinary retention. It usually goes away over time without treatment.
Due to the low effectiveness of therapy and the high likelihood of complications, surgical treatment methods are rarely resorted to. Urologists strive to cure prostatitis without surgery.
Prevention of prostatitis
To prevent the occurrence of prostatitis, men after 30 years of age should engage in disease prevention.
Methods of primary prevention aimed at preventing the disease include:
- Regular exercise, especially for those who have a sedentary job or a sedentary lifestyle. Running, swimming, tennis are recommended.
- It is important to have regular sex life to activate blood flow in the pelvic organs and increase tone.
For people who have already had prostatitis once, secondary prevention measures are recommended:
- Regular examinations with a urologist and undergoing examinations for early detection of recurrent signs
- Drug therapy.
Important! Medicines should only be prescribed by an experienced specialist. Self-medication is unacceptable.
All representatives of the stronger sex should be attentive to their health. If unpleasant symptoms appear, you should definitely seek medical help.
Often men are embarrassed to go to the doctor, but this only aggravates the situation and aggravates the course of the disease. After all, prostatitis can provoke other dangerous conditions: adenoma, varicocele, cancer.
Remember: the later you go to the doctor, the longer it will take to treat the identified pathology.
Source: https://UroMir.ru/vospalenie/terapija/operaciya-prostatita-u-muzhchin.html
Surgical treatment of prostate adenoma
Benign hyperplasia (proliferation) of prostate tissue or prostate adenoma is one of the most common genitourinary diseases in men. 11.3% of them after 40-49 years suffer from this disease. In the early stages, conservative treatment can stop it, but then only surgery and laser vaporization can help the patient.
Causes and diagnosis of prostate adenoma
BPH
Prostate adenoma is a benign enlargement of prostate cells. In most cases, this disease affects men over 50 years of age.
It is dangerous because it can transform into cancer.
The pathology interferes with the release of sperm-forming fluid and disrupts the functioning of the bladder (after all, part of the urethra passes through the prostate, which is compressed as the gland grows).
Experts believe that the main cause of prostate adenoma is age-related hormonal imbalance, an increase in the level of testosterone, hydrotestosterone, and a decrease in the amount of other sex hormones, which negatively affects prostate cells.
Symptoms You Shouldn't Ignore
- Frequent urination at night and during the day, the process occurs with difficulty, the stream of urine is interrupted or weakened. These are manifestations of stage 1 of the disease, when the functions of the bladder and kidneys are preserved. At this stage, the progress of the disease can be stopped.
- Feeling of an unemptied bladder; you have to strain when urinating. This is how stage 2 of the disease develops. Now the organ’s capabilities have been exhausted, and it cannot fully cope with its functions.
It is important to remember that symptoms in men rarely appear at the same time, and there may be a significant period of time between them. If at least one suspicious sign appears, you should definitely contact a urologist for consultation.
Due to increased pressure in the urinary system, the functioning of the kidneys is disrupted, the inflammatory process begins, complications appear: hemorrhoids, pyelonephritis, inguinal hernias, urinary retention, atony of the bladder, when it loses its tone and cannot excrete urine.
- Feeling of discomfort in the perineal area, the influence of chronic urinary retention, renal failure (stage 3).
- Pain after urination, ejaculation.
These signs are a direct indication for starting treatment. To assess the stage of development of the pathology, the specialist will conduct a rectal examination (palpation of the prostate through the wall of the rectum to determine its structure, soreness) and prescribe a blood test to determine the level of PSA - a prostate-specific antigen or cancer marker. Normally, its value does not exceed 4 ng/ml.
TRUSY
At the next stage, the patient undergoes an ultrasound of the prostate and determines the volume of residual urine. TRUS is considered the most informative ultrasound method for diagnosing prostate adenoma, which makes it possible to fully assess the structure of the gland (the examination is carried out through the rectum, transrectally). It is important to remember that the symptoms of the disease do not always manifest themselves comprehensively and may disappear temporarily.
Based on the data obtained, the doctor determines the tactics for eliminating prostate adenoma: medication or surgery. In the first case, it is possible to reduce the size of the pathology and normalize the functioning of the bladder. The second approach is used if conservative therapy is ineffective and there are complications. Types of surgical treatment can be divided into 2 categories:
- transurethral resection of prostate adenoma (TUR): removal is performed without incisions of the skin through the urethra, indications are narrowing of the urinary tract, the size of the enlarged gland does not exceed 80-100 cm³. Transurethral resection of the bladder is performed using the same technology;
- laser vaporization (excision of tissue with a laser under the influence of high temperature - up to 80°);
- transvesical removal of the prostate: this is an abdominal operation, it is prescribed, as a rule, in advanced cases, in the presence of complications; in some cases, the intervention involves the application of an epicystostomy - a special tube through which urine will be drained.
In advanced cases, only complete removal of the prostate gland can help.
Advice: after 50 years, every man should take a blood test for PSA once a year to monitor its level and visit a urologist, so that in case of asymptomatic development of oncopathology, it can be eliminated in a timely manner.
Identifying prostate disease at an early stage ensures effective treatment and minimizes the chances of developing cancer. Otherwise, only surgery to remove prostate adenoma will bring a positive result.
The importance of the PSA parameter in diagnosing adenoma
PSA is a special protein that is produced by the prostate and helps create a favorable environment for sperm to move through. But it also enters the blood, so its level can be determined in the laboratory. The antigen is directly related to the size of the gland and as it increases, its quantity increases.
Using this analysis, men can be diagnosed not only with adenoma, but also with prostate cancer (in the latter case, the norm will be exceeded - 20 ng/ml).
Oncology can only be definitively confirmed by transrectal sampling of gland tissue, which is carried out under ultrasound guidance.
Preparation for a prostate biopsy includes taking a blood test, urine test, not taking certain medications, and taking an antibacterial drug to prevent inflammation.
But in most cases, an increase in the amount of this substance is associated with inflammation or adenoma.
Advice: it is important to know that PSA levels in men increase not only in the case of adenoma or cancer. Several factors contribute to this: inflammation in the prostate, its massage, recent ejaculation, prolonged cycling. A blood test for free PSA (not bound to proteins) is more informative and accurate: the lower its level, the higher the likelihood of a tumor.
Methods of surgical treatment of prostatic hyperplasia
TOUR of prostate adenoma
The initial goals of treatment for men with BPH are to relieve urinary tract symptoms, improve quality of life, and prevent complications.
To do this, they are offered drug therapy based on alpha-blockers, 5-alpha reductase inhibitors, and herbal preparations.
But sometimes only surgery can help a person.
Abdominal surgery is rarely performed if there is no safe alternative method (indications: stones, tumors, diverticula or protrusion of the bladder wall), or if the adenoma is large.
But in small towns, in the absence of specialists who possess the necessary technologies and equipment, interventions using this technology are still carried out, including open operations to remove stones from the gall bladder.
Modern medicine has less traumatic and more effective methods of surgical treatment.
- Monopolar electrosurgery - transurethral laser vaporization (removal of the prostate gland is done using an endoscopic resectoscope instrument and roller electrodes: they remove the affected tissue, which is evaporated with a powerful high-frequency current);
- Transurethral resection, TUR (performed endoscopically, that is, through the organ cavity without incisions or opening the bladder, its effectiveness is estimated at 80%). The doctor inserts a resectoscope with a diathermocoagulator at the end into the urethra, which is used to excise the affected prostate tissue, after which the edges of the wound are cauterized. The removed fragments are washed out with a special irrigation liquid;
- Laser methods:
- visual laser ablation of the prostate (the laser removes the affected tissue and expands the lumen of the urethra);
- interstitial laser coagulation (energy is directed to the adenoma using a flexible optical fiber; high temperature destroys cells and forms scars, which improves the flow of urine);
- transurethral thermotherapy (with the help of microwaves the tissue is evaporated, the size of the adenoma is reduced, but the effect is temporary);
- transurethral radiofrequency thermal destruction (thermal energy thermally damages the prostatic urethra from the neck of the bladder to the prostate tissue adjacent to the urethra; after removing dead cells in 4-6 weeks, a cavity is formed at the site of the intervention, eliminating blockage of the urinary tract);
Laser vaporization (works on the basis of infrared rays that vaporize tissue) is a worthy alternative to transurethral resection.
To treat men with cancer, surgical, drug, hormonal, radiation, and chemotherapy are used. If you pay attention to the symptoms of prostate pathology, you can avoid this difficult treatment.
Complications and consequences of pathology
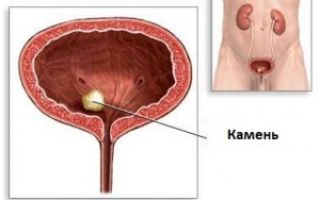
Bladder stone
If you do not eliminate the disease, it can cause complications in the functioning of other organs. Most often, these are disturbances in the functioning of the bladder, the formation of stones in it, repeated inflammatory processes in the genitourinary system, hematuria - the presence of blood in the urine, dilatation of the upper urinary tract.
The consequences of surgery to remove prostate adenoma depend on the chosen method and the stage of the disease. The rates are much higher in the case of open surgery and much lower in TURP.
It is transurethral resection that is considered the “gold standard” in the surgical treatment of prostate adenoma.
After this type of operation, TUR syndrome may occur, caused by the entry of fluid, which washes out fragments of dead tissue, into the blood, damage to neighboring organs, and disruption of the properties of the blood.
Patients may also experience bleeding, injuries to the urethra, sphincter, infectious and inflammatory processes, urinary incontinence, and exacerbation of chronic diseases. Complications from cancer reduce the success of surgery and negatively affect life expectancy. Full rehabilitation after prostate surgery cannot be carried out without antibiotic therapy, nutritional correction, and physical rest.
Surgical treatment methods and laser vaporization make it possible to effectively remove affected tissues with minimal harm to the body. To prevent prostate cells from degenerating into cancerous ones, you need to undergo preventive examinations with a urologist and begin the fight against the disease in the early stages, when the symptoms are not yet so pronounced.
We recommend reading: surgery to remove varicocele
Video
Attention! The information on the site is presented by specialists, but is for informational purposes only and cannot be used for independent treatment. Be sure to consult your doctor!
Source: https://vseoperacii.com/mps/predstatelnaya-zheleza/lechenie-adenomy.html
Surgical treatment of prostate adenoma: types and their description
Benign prostatic hyperplasia or prostate adenoma is one or more nodules that tend to grow and increase in size over time.
Hello, Alexander Burusov is here, an expert at the Viva Man men’s club. Today we will talk about surgical methods for treating prostate adenoma.
This disease is not considered uncommon among males over fifty years of age. And surgical treatment of prostate adenoma is the most common and most effective method that is available in our time to combat this disease.
Indications for surgery
In order for a surgeon to prescribe surgical treatment for prostate adenoma, the patient must have certain signs:
- systematic increase in the volume of residual urine;
- infection with sexually transmitted diseases;
- recurrent urinary problems;
- a large volume of red blood cells in the urine;
- large saccular protrusions of the intestinal walls;
- urinary signs of the disease that cannot be relieved by traditional methods;
- progressive development of kidney diseases associated with the functioning of the bladder;
- the presence of postoperative bleeding caused by tumor enlargement, which cannot be cured with medications.
Contraindications to surgery: various chronic and acute diseases of the kidneys or bladder, which are in the stage of an inflammatory process or chronic; protrusion of the walls of the aorta; absolutely any pathology associated with the work of the heart; atherosclerosis of cerebral vessels.
Types of operations
Surgical treatment of prostate adenoma quite often becomes the last opportunity to find a solution to a painful problem associated with getting rid of an ill-fated tumor, as well as an opportunity to significantly improve your life.
Urologists note that surgery for prostate adenoma firmly holds the silver medal in terms of frequency. And the statistics are merciless - 30% of patients complete their treatment by resorting to surgery.
The choice of a specific type of operation depends on many factors. The main ones are: tumor size; age characteristics of patients; the presence and severity of other diseases present at the time of diagnosis; technological equipment of the hospital and the degree of qualification of personnel.
Open adenomectomy
Thirty years ago, such surgical intervention was considered one of the most effective. Surgical treatment of prostate adenoma in this case comes down to the following.
First, the stomach is cut, and it does not matter whether this cut is transverse or longitudinal. The choice of incision method depends entirely on the personal preferences of the operating surgeon.
After this, the anterior wall of the bladder is cut. The urologist examines the internal condition of the bladder for the presence of stones, saccular formations on the walls, and other neoplasms.
After this, the doctor uses his finger to remove the tumor itself, blocking the urethra. To successfully carry out such actions, the specialist must have a wealth of experience and dexterity so as not to cause irreparable harm to the patient.
After the tumor is removed, the patient is sutured and the catheter is removed from the urethra. The postoperative period after removal of prostate adenoma is no more than a week, during which the patient is inpatient treatment in the clinic under the supervision of specialists.
Indications for open adenomectomy: the size of the tumor must exceed 80 grams, patients may have urinary bloating, and there are also pathological changes in the urinary organs.
The disadvantage of this method is the presence of urinary incontinence in patients within 6-7 weeks after surgery. The most common complications: heart attack, pulmonary embolism, blood clots, increases the risk of stroke.
Transurethral resection (TUR)
Transurethral resection of prostate adenoma is the “gold standard”, recognized by leading urologists as a treatment for this type of tumor.
Surgery to remove prostate adenoma using transurethral resection is prescribed for patients whose tumor size at the time of diagnosis is no more than 80 grams, and also if the duration of the operation is no more than sixty minutes.
In case of suspicion of a malignant nature of the tumor or its larger size, the above type of operation is chosen. Upon completion of transurethral resection of prostate adenoma, reviews and ratings are at a very high level. In particular, up to ninety percent of all patients note a sharp change in the picture towards improvement.
Transurethral resection of prostate adenoma is an operation associated with complete or partial disposal of tumor cells using a device inserted through the urinary tract - a special loop. When performing this operation, a cystoscope is also used, which allows you to see and guide the progress of the operation and the actions of the attending surgeon.
After surgery for prostate adenoma, as in the first case, the patient is given a catheter. The postoperative period after removal of prostate adenoma using transurethral resection is 2 days and, accordingly, he will be in the clinic for only two days.
Patients are also advised to watch out for constipation for about seven weeks, try to minimize physical activity, and also be patient with sexual intimacy.
Laparoscopy
Laparoscopy is characterized by minimal intervention in the patient's body. When laparoscopy is performed, small holes are made in the abdomen into which surgical instruments and a micro-sized video camera are inserted.
Watching on the screen, the surgeon uses an ultrasonic knife to remove the affected areas of the prostate gland, causing the minimum possible damage to healthy ones. After surgery for prostate adenoma, the catheter remains with the patient for six days.
Electrovaporization of the prostate gland
This method has great similarities with transurethral resection. The only difference is that with electrovaporization the current in the loop is 290 watts. This power reduces the risk of postoperative bleeding.
This is due to the fact that the loop instantly coagulates the walls of blood vessels. This approach contributes to the increasing popularity of this method of surgical treatment.
Laser resection
Just like laparoscopy, it is a minimally invasive type of surgery. To carry it out, lasers with different wavelengths are used.
The tumor cells are exposed to a green laser beam. This process lasts as long as it takes to bring the contents of the tumor cells to a boil, after which the tumor parenchyma is destroyed.
This operation to remove prostate adenoma is good because there are either no complications after it, or their rate is close to zero. This refers to the following complications after surgery: bleeding, ejection of sperm in the opposite direction, impotence and incontinence, and at first patients may experience a slight burning sensation after urination or incontinence.
Transurethral needle ablation
The attitude of specialists towards an operation called transurethral needle ablation is very ambiguous . This is due to the fact that there is no evidence of a long-term effect from it. The essence of the method is to expose the affected cells to high-frequency radio waves, which contribute to its thermal damage.
The operation of prostate adenoma in the form of transurethral needle ablation is considered quite simple. It is so easy to perform that it is performed under local anesthesia and after surgery for prostate adenoma, patients do not always need a catheter.
Prostate adenoma is a terrible diagnosis for a man, but this problem can be easily dealt with if you do not neglect the disease, which has serious consequences.
Price policy
The cost of surgery to remove prostate adenoma varies depending on the region of the country and the type of surgery. For example, transurethral resection costs approximately from six to one hundred and twenty thousand rubles.
The average cost is 30-60 thousand. The cost of open adenomectomy ranges from 15 to 100 thousand, but if you take the optimal price-quality ratio, it will cost 50 thousand rubles.
And the price for laser resection ranges from fifty to one hundred thousand rubles. If we take the optimal ratio, then it will be possible to do it for 80 thousand rubles.
Source: http://viva-man.ru/adenoma-prostaty/hirurgicheskoe-lechenie-adenomyi-prostatyi/
Types of surgery for prostate adenoma
Despite the availability of a significant number of methods of conservative treatment of prostate adenoma. Only surgical treatment is radical.
Indications for surgery
Indications for surgical treatment depend on the stage of prostate adenoma. the appearance of residual urine, persistent infection, recurrent attacks of urinary retention, hematuria, multiple stones in the space behind the prostate, a sharp increase in nighttime urination that disrupts sleep - all these symptoms indicate the need for surgery.
Contraindications
Contraindications to simultaneous adenomectomy are severe forms of renal (azotemia, hypoisosthenuria) or heart failure, aortic aneurysm, advanced forms of cerebral atherosclerosis, cor pulmonale.
Exacerbation of chronic pyelonephritis and cystitis is also a contraindication. Many of these contraindications are temporary, and the patient can be prepared for surgery with appropriate treatment.
In order to prevent postoperative embolism, it is necessary to identify and treat varicose veins of the lower extremities; if any, it is recommended to bandage the lower extremities with an elastic bandage in the preoperative period, during the operation and in the postoperative period.
Types of operations
The following types of surgical treatment are used.
1. Two-stage transvesical surgery according to Holtsov. This operation is indicated for weakened patients with poor renal function when long-term drainage of the urinary tract is required.
The first stage of the operation is the application of a suprapubic fistula for the period necessary to improve kidney function (from 3 weeks to 6 months).
The second stage of the operation is transvesical enucleation of the adenoma. The disadvantage of this type of operation is the need to leave drainage for a long time.
2. Simultaneous transvesical adenectomy according to Fedorov-Freyer. This operation is characterized by its simplicity of approach; its mortality rate is about 2%. It is supplemented by a number of techniques aimed at ensuring hemostasis by suturing the edges of the prostatic bed or suturing it.
Hemostasis during this operation is also ensured by the use of a catheter with a Pomerantsev-Foley type balloon. Reduced blood loss leads to a reduction in postoperative complications such as renal failure or sepsis.
3. The operation according to the Harris-Grinchak method consists of suturing the prostatic bed after adenomectomy under eye control around a previously inserted catheter: after removing the tissue remaining after enucleation, sutures are applied to the edges of the prostatic bed with a significantly curved needle on a long needle holder.
If the bleeding has completely stopped, the bladder can be sutured tightly; A small rubber or gauze graduate is inserted into the lower corner of the wound for 2 days. An indwelling catheter ensures urine evacuation for 10 days.
This method gives good results with careful postoperative care, especially in the first 2 days after surgery: every 2 hours the bladder is washed with warm isotonic sodium chloride solution or 3.8% sodium citrate solution to prevent the formation of blood clots.
4. Retropubic adenomectomy was first proposed by A. T. Lidsky and developed by T. Millin. This operation competed with Harris' operation for a long time. Currently, it is used less frequently due to observed complications - up to 15%.
The patient is placed in the Trendelenburg position with legs apart; The prostate gland is approached through a vertical or transverse suprapubic incision.
The peritoneal transitional fold is retracted upward; the retropubic tissue is carefully retracted downwards and laterally, avoiding exposure of the posterior surface of the pubic joint. The large veins lying in the fascia on the anterior side of the prostate gland are divided between the ligatures.
The prostate capsule is opened with a transverse incision 1 cm below the bladder neck.
The prostate adenoma is removed from the capsule partly with long curved scissors, partly with a finger, highlighting it right up to the wall of the bladder; By crossing the central part of the urethra at the very neck of the bladder, the tumor is removed.
To prevent obstruction after adenomectomy, a cuff of the mucous membrane is excised from the posterior arch of the bladder neck.
Hemostasis is ensured by diathermy, as well as by applying a permanent suture to the wound in the prostatic capsule; the latter is very important.
After careful hemostasis, a catheter No. 18-22 with large holes at the end is inserted through the urethra into the bladder. The wound is sutured layer by layer over the catheter, and a rubber release is inserted into its lower corner for 48 hours.
The bladder is washed with hot saline and filled with a 3.8% solution of sodium citrate for 1 hour.
5. Perineal adenomectomy according to Young is currently almost never used due to the risk of complications: urinary incontinence, perineal fistulas, impotence. The occurrence of these complications with the perineal approach is quite understandable, since the adenoma is removed through the caudal zone of the prostate, which is closely connected with the tissues of the external sphincter.
6. Transurethral resection of the prostate is often performed using the electrosurgical method; It is used for disorders of the outflow of urine from the bladder caused by prostate adenoma or cancer, sclerosis or a tumor of the bladder neck.
Contraindications to transurethral resection:
- narrowing of the urethra, preventing the possibility of passing the instrument into the bladder,
- insufficient bladder capacity,
- severe renal failure.
Transurethral electroresection can be performed under local infiltration anesthesia according to A. V. Vishnevsky, intravenous or inhalation anesthesia. The operation consists of excision of tissues narrowing the neck of the bladder; It is performed with a special instrument - a resectoscope.
It is an endoscopic device equipped with a movable loop-shaped electrode, with the help of which semi-cylindrical pieces of pathological tissue are cut off. Electrical resection is carried out under a continuous flow of fluid through the flushing system.
For this purpose, it is recommended to use isotopic solutions of glucose and urea.
Operation technique: a resectoscope with an obturator is inserted into the bladder; the obturator is removed, and after partial filling of the bladder, an electrode and an optical system are inserted in its place; connect the inputs of the lighting and coagulating current, as well as the flushing system; The high-frequency current is turned on (by the operator or assistant) using a foot pedal at the moment of reverse movement of the electrode. The cut tissue cylinders are removed by a reverse flow of liquid.
In case of significant bleeding, the bleeding areas are coagulated using a special roller electrode. To achieve a positive result, make from 10 to 50 sections. After electrical resection, a permanent balloon catheter is inserted into the bladder for 3-7 days, through which the bladder is washed 3-4 times a day.
The most common complication of transurethral resection is bleeding. In addition to electrocoagulation, blood transfusions are used for hemostasis; in more severe cases, epicystostomy with cervical tamponade or adenomectomy may be necessary.
To prevent bleeding, it is recommended to use local hypothermia by cooling the washing fluid (to t° +2°) with the addition of vasoconstrictors (adrenaline, norepinephrine).
When using distilled or boiled water to fill and rinse the bladder, electrolyte imbalances and intravascular hemolysis may occur.
Cases of oliguria and anuria have been described.
Errors in the surgical technique can lead to perforation of the bladder wall; in this case, there is a discrepancy between the amount of injected and outflowing fluid during lavage of the bladder.
If the operation is performed under local anesthesia, the patient experiences acute pain in the lower abdomen when the bladder wall is perforated. Treatment of this complication: urgent application of a suprapubic fistula with drainage of the paravesical space.
If intra-abdominal perforation is suspected, a revision of the abdominal cavity is indicated.
After transurethral electroresection, in case of damage to the external sphincter of the bladder, urinary incontinence sometimes occurs, which may require complex plastic surgery.
Since 1964, the method of cryosurgery of the prostate gland has become widespread. Using a special instrument, the prostate gland containing adenomatous or cancerous nodes is frozen.
The most widely used cryothermal device is the Linde CE-4 cryosurgery system. Its main part is a special cryoprobe, mounted in the form of a catheter No. 25 according to Charrière, in which liquid nitrogen circulates.
The working freezing surface corresponds to the prostatic part of the urethra, and the non-working surface is isolated in such a way that the risk of freezing of other parts of the urethra and bladder is reliably eliminated.
Cryodestruction usually occurs at temperatures from -120 to -190° for 2-5 minutes.
After applying cold for 2 days, the stage of acute edema develops. Then, within a week, there is a stage of coagulative necrosis with cell autolysis, and then a healing stage - from 3 to 6 months.
Considering that the main disadvantage of cryoprobes is the impossibility of using them under visual control, N. J. Reuter proposed visual control using a special trocar cystoscope inserted into the bladder by suprapubic puncture.
Cryosurgery is indicated for seriously ill patients who are contraindicated for adenomectomy or transurethral resection (approximately 5-10% of cases). With prostate cryosurgery there may be complications: late bleeding, pyelonephritis, urethral fistulas, osteitis of the pubic bones.
Postoperative complications of adenectomy
In the postoperative period, complications may arise with all types of surgical interventions.
Pulmonary embolism is especially dangerous. Getting up early helps prevent this complication. Secondary septic bleeding from the prostatic bed is a serious postoperative complication. It usually occurs on the 7-10th day after surgery. On the 2-3rd day after adenectomy, the urine is cleared of blood.
If this does not happen and the blood admixture remains on the 4-5th day, then this indicates an inflammatory process in the bed; the latter may be the cause of septic bleeding.
If rinsing the bladder with hot isotonic sodium chloride solution or silver nitrate solution does not stop bleeding, bed tamponade and blood transfusion are indicated.
Fever in the first days after surgery often accompanies adenomectomy. A prolonged increase in temperature to 38-39°, stunning chills indicate pyelonephritis or thrombophlebitis in the space near the prostate. In these cases, treatment with antibiotics and chemotherapy is necessary. Stricture of the posterior urethra develops in 3-6% of cases.
It is quickly eliminated by bougienage. Urinary incontinence does not occur with correctly performed transvesical adenomectomy. The development of this complication indicates damage to the caudal part of the prostate gland and the fibers of the external sphincter; long-term treatment with bougienage, lavage of the bladder in the immediate postoperative period, and later physiotherapy are required.
prostate massage.
Long-term non-healing suprapubic urinary fistulas require excision with layer-by-layer suturing of tissue.
The occurrence of osteitis pubis (osteochondritis, aseptic osteonecrosis, panostitis) - localized osteoporosis of the pubic bones - is associated with the combined effects of trauma, neurotrophic disorders in the pelvic bones, leading to their demineralization. Osteitis manifests itself as sharp pain in the symphysis pubis and upper thighs.
In the postoperative period for osteitis pubis, bed rest and long-term use of corticosteroids (prednisolone 0.005 g 2-4 times a day, dexamethasone 0.001 g 2-3 times a day) in combination with antibiotics are recommended.
The results of treatment of prostate adenoma have improved significantly in recent years. Suprapubic adenomectomy is the main and most common surgical method. Many urologists and surgeons recommend expanding the indications for simultaneous surgery.
Mortality with it is 3%. Retropubic adenomectomy in our country has gained little popularity due to complications: thrombosis, fistulas and osteitis pubis, which is observed in 0.5-2% of those operated on. The mortality rate for this operation ranges from 3% (E. Sh.
Savich) up to 6% (V. Borcher).
Transurethral electroresection is a significant advance in the surgical treatment of prostate adenoma, but it can be used in a limited number of patients with small intravesical and intraurethral adenoma.
There are complications with this intervention, especially bleeding and inflammation.
The low mortality rate of this operation (0-2%) and the ability to use it in weakened old people and people suffering from cardiovascular diseases encourage us to recommend wider use of this method.
The causes of mortality for all methods of adenomectomy have changed significantly: if in the period from 1931 to 1948.
the main cause of death was urinary infection and its complications, then over the past 10-15 years the main cause of postoperative mortality has been thrombosis and embolism of cerebral and pulmonary vessels, as well as cardiovascular failure. Overall mortality for all methods of adenomectomy has decreased significantly and continues to decline.
The progressive decrease in mortality is explained not only by the successful fight against infection, but also by careful preparation of patients with cardiovascular and other diseases for surgery, the correct choice of time and method of surgery, the prevention of thromboembolism, and careful postoperative care.
Source: http://therapycancer.ru/rak-predstatelnoj-zhelezy/1075-tipy-operatsii-pri-adenome-predstatelnoj-zhelezy